Total Knee Replacement (Arthroplasty)
Comprehensive knee joint replacement to relieve pain and restore mobility
Total Knee Replacement, also known as Total Knee Arthroplasty, is a well-established surgical procedure used to treat advanced knee joint degeneration. This surgery may be considered when chronic pain, stiffness, or reduced mobility from conditions such as osteoarthritis, rheumatoid arthritis, or previous injury begins to interfere with daily life and conservative treatments are no longer effective. During the procedure, the damaged surfaces of the knee joint are carefully removed and replaced with artificial components (prostheses) made from durable materials such as metal, ceramic, or high-grade plastic. These implants are designed to restore smoother movement, improve stability, and reduce or eliminate the pain associated with joint deterioration.
At Melbourne Orthopaedic Clinic, our surgeons use a range of advanced surgical systems to tailor each knee replacement to the individual patient. These include robotic-assisted techniques, patient-specific instrumentation (PSI), kinematic alignment(KA), and augmented reality platforms. By using these technologies, your surgical plan can be precisely matched to your unique anatomy and functional goals.
On this page, you will learn about:
- Signs it may be time for a knee replacement
- An overview of the total knee replacement surgical techniques
- The knee replacement implant components
- Potential benefits of total knee replacement
- How to prepare for your knee replacement surgery
- Your total knee replacement surgical procedure
- Recovery after total knee replacement
- Risks and complications to be aware of
- Adjusting to life after a total knee replacement

Signs it may be time for a knee replacement
Choosing to undergo total knee replacement surgery is a major decision, typically considered after other non-surgical treatments have not provided adequate relief. If knee pain or stiffness is starting to affect your ability to enjoy everyday life, recognising the signs that surgery may be appropriate can help guide your next steps.
- Ongoing knee pain that limits your lifestyle – Persistent pain that continues despite rest, medication, or physiotherapy is one of the most common indicators. If knee pain is stopping you from walking, working, exercising, or sleeping comfortably — or if you find yourself relying more on pain relief — it may be time to consider surgical options.
- Loss of mobility and knee stiffness – Struggling with basic movements like getting out of a chair, climbing stairs, or walking short distances could suggest advanced joint damage. Morning stiffness, or a knee that feels increasingly difficult to bend or straighten, may mean the joint is no longer functioning as it should.
- Visible changes in your knee – Changes such as swelling, deformity (e.g. bow-legged or knock-kneed appearance), or a sensation that the knee is giving way or buckling under your weight can be signs of structural deterioration that may not be reversible without surgery.
- Conservative treatments no longer working – When options like exercise, weight loss, physiotherapy, joint injections, or anti-inflammatory medications stop providing relief, it may indicate that joint degeneration has progressed too far for non-surgical treatments to remain effective.
- Advanced arthritis on imaging – If X-rays or other scans show significant damage caused by osteoarthritis, rheumatoid arthritis, or post-traumatic arthritis, knee replacement surgery may be the most reliable option to reduce pain and improve long-term joint function.
Recognising these signs is the first step in considering knee replacement surgery. The decision is, however, personal and depends on how your symptoms affect your quality of life.
An overview of the total knee replacement surgical techniques
Total knee replacement surgery continues to evolve, with modern surgical techniques offering greater precision, better alignment, and the potential for faster recovery. At Melbourne Orthopaedic Clinic, our surgeons draw on a wide range of proven and emerging technologies to tailor each procedure to the individual. The goal is to relieve pain, restore joint function, and support long-term mobility through a personalised approach.
This well-established technique involves placing the knee implant in a straight, neutral position, typically perpendicular to the mechanical axis of the leg. It remains a widely used method that may be suitable for patients with severe deformities caused by arthritis or trauma. Mechanical alignment aims to evenly distribute forces across the joint and enhance long-term implant durability.
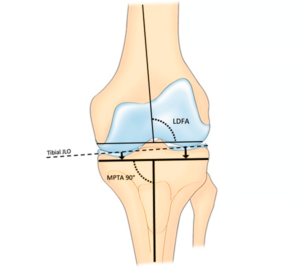
Kinematic alignment is a more personalised technique that aims to match the natural shape and motion of your knee before it was affected by arthritis. By preserving your natural joint line and soft tissue balance, this method may feel more natural during movement and daily activities.
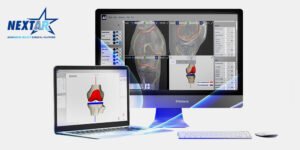
Robotic-assisted knee replacement surgery uses advanced systems such as Mako SmartRobotics™ or Zimmer ROSA to support precise planning and implant positioning. These technologies help your surgeon tailor the procedure to your individual anatomy, with the goal of improving alignment, function, and early recovery.

Before your procedure, a CT or MRI scan can be used to design 3D-printed surgical guides tailored to your unique anatomy. These custom cutting guides help the surgeon make accurate bone cuts and implant placement decisions during surgery. PSI can be particularly useful in patients with unusual anatomy or complex joint changes.

Computer-assisted surgery (CAS) uses advanced imaging, such as CT or MRI scans, alongside navigation technology to guide your surgeon during the procedure. In some cases, augmented reality (AR) tools are also used to overlay digital information onto the surgical field in real time. These technologies support accurate bone preparation and precise implant placement, which may contribute to better alignment, function, and long-term results.
At Melbourne Orthopaedic Clinic, no two knee replacements are the same. Your surgeon will carefully select the most appropriate surgical approach and technologies based on your diagnosis, joint alignment, bone structure, and personal goals. Whether your procedure involves robotic assistance, kinematic alignment, augmented reality, or traditional methods, each technique is used to support a safe operation and successful recovery.
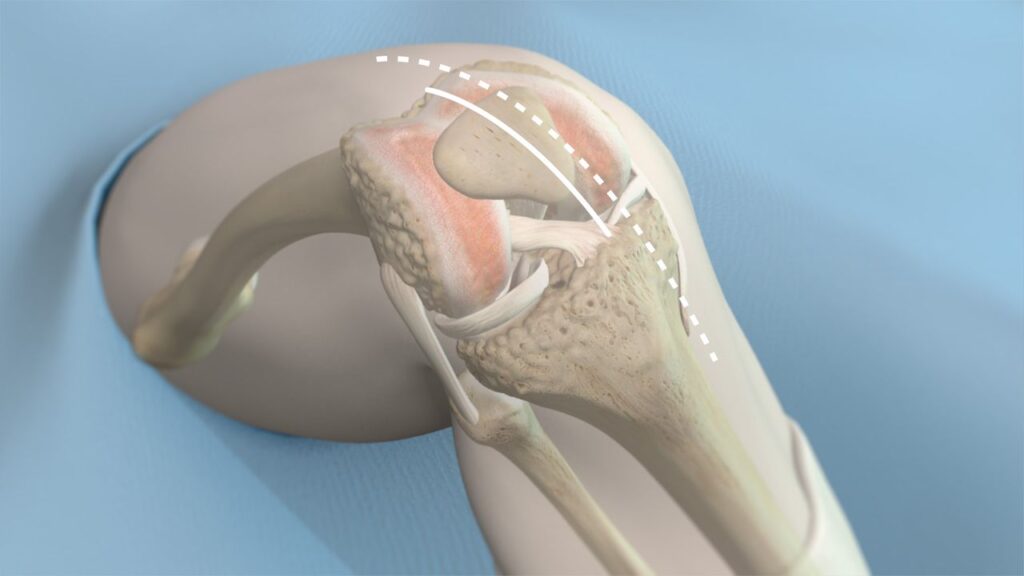
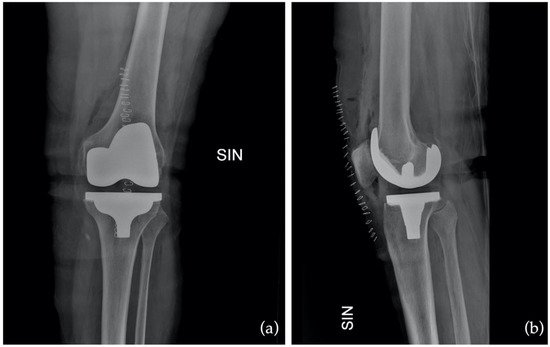
The knee replacement implant components
During a total knee replacement procedure, damaged bone and cartilage are replaced with prosthetic components that mimic the function of your natural joint. These components are carefully selected to restore mobility, stability, and comfort, tailored to your unique anatomy and lifestyle needs.
Knowing the basic structure and function of a knee implant can help you better understand what’s involved in your surgery and what contributes to the success of the outcome.
The femoral component is made of metal (usually a cobalt-chromium or titanium alloy) and is shaped to match the contours of the end of your thigh bone (femur). It curves around the front of the knee and fits into a groove that allows your kneecap (patella) to glide smoothly as the knee moves. This component bears much of the load during walking, squatting, or bending and must be precisely aligned to allow for smooth flexion and extension of the knee.
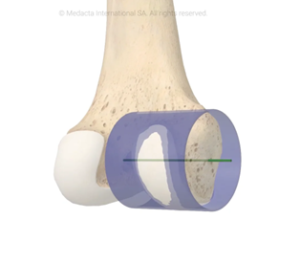
The tibial component consists of two parts:
Tibial baseplate: A metal platform fixed to the top of your shin bone (tibia) using either bone cement or a press-fit technique.
Tibial insert: A high-grade plastic spacer (made of ultra-high-molecular-weight polyethylene) that sits atop the baseplate.
This plastic insert functions like your knee’s natural cartilage. It cushions the joint, absorbs shock, and allows the femoral component to glide smoothly over the tibial surface. Modern inserts are engineered to be wear-resistant and may include antioxidant-enhanced materials such as Vitamin E to improve durability. In some cases, if only the plastic insert wears out over time, it can be replaced without disturbing the metal implants.
Not all knee replacements require resurfacing of the patella (kneecap), but when it is involved, a small plastic dome is attached to the underside of your kneecap. This enables it to move more smoothly over the femoral component during knee bending and straightening.
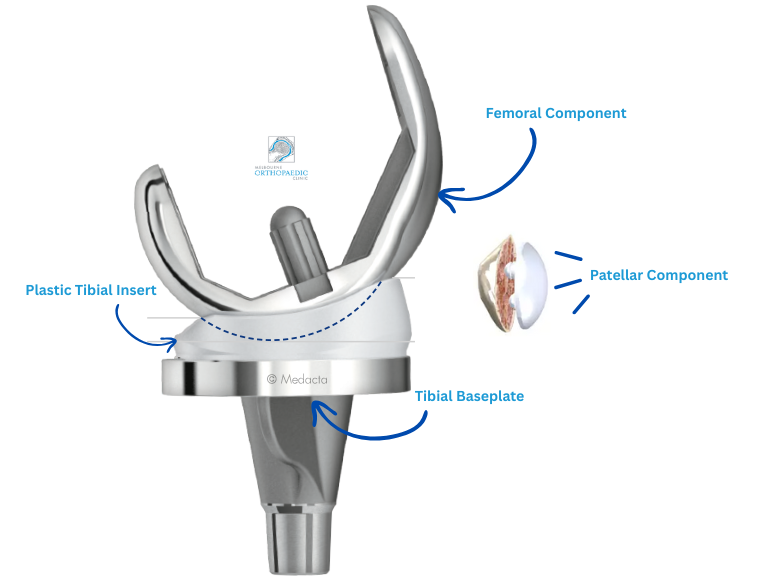
Implant materials and durability
Knee implants are typically made from a combination of cobalt-chrome or titanium alloys, and high-grade polyethylene (plastic). These materials are biocompatible, which means they are designed to function safely within your body. Modern implant designs and materials aim to reduce wear and extend the life of the replacement. Your surgeon may select either a fixed bearing or mobile bearing implant design
The choice of implant materials, sizes, and design features is determined by several factors including your bone quality, activity level, and the alignment of your knee. During pre-operative planning, imaging such as X-rays, CT, or MRI scans help your surgeon select and position the components to match your natural anatomy.
At Melbourne Orthopaedic Clinic, your surgeon will select a prosthesis from a range of well-established implant systems known for their safety, performance, and long-term outcomes.
Fixed bearing designs have a polyethylene insert locked into the tibial baseplate. This is the most commonly used type and is suitable for many patients.
Mobile bearing designs allow some movement between the insert and the baseplate, which may offer better rotation for selected patients.

Potential benefits of total knee replacement
Knee replacement surgery at Melbourne Orthopaedic Clinic is performed to relieve pain and improve function in knees affected by arthritis, injury, or long-term wear and tear. It involves replacing damaged joint surfaces with prosthetic components designed to restore smoother movement and stability. Potential benefits of knee replacement surgery include:
Pain reduction – Knee arthritis can cause persistent discomfort that affects daily life. Many people considering surgery are seeking relief from chronic pain that hasn’t improved with non-surgical treatments.
Improved mobility – By resurfacing the worn or damaged areas of the joint, knee replacement may help restore your ability to walk, climb stairs, and move with greater ease.
Better joint alignment – In cases where arthritis has altered the natural alignment of your leg, surgery may assist in correcting deformities and improving joint structure.
Return to daily activities – With less pain and improved joint function, you may be able to return to activities that had become difficult or were avoided altogether.
Durable, long-term results – Modern implants are designed to offer long-lasting function when paired with rehabilitation and ongoing care.
Personalised advice for your situation
Recovery after knee replacement is a gradual process that requires physiotherapy and post-operative support. During your consultation at Melbourne Orthopaedic Clinic, your surgeon will assess your knee condition, discuss your goals, and explain whether surgery is appropriate for your needs. You’ll also receive guidance on the type of procedure, implant options, and expected recovery timeline.
How to prepare for your knee replacement surgery

Being prepared for knee replacement surgery can make a meaningful difference to both your surgical experience and your recovery. Taking proactive steps before your procedure can help you feel more at ease, support your rehabilitation, and set the stage for the best possible outcome. Here’s how to prepare for your knee replacement surgery at Melbourne Orthopaedic Clinic.
Before undergoing knee replacement surgery, you’ll attend a comprehensive consultation with your Melbourne Orthopaedic Clinic, orthopaedic surgeon. This appointment is designed to assess your knee condition, understand your overall health, and tailor a surgical plan to your specific needs.
What to expect during your consultation:
Review of your medical history: Your surgeon will discuss your past and current medical conditions, medications, allergies, and any previous surgeries. This information helps identify potential risks and ensure a safe surgical plan.
Physical examination: A thorough examination of your knee will be performed to assess joint function, range of motion, and the extent of damage.
Imaging tests: You may be referred for X-rays, MRI, or CT scans to obtain a detailed view of your knee joint. These images assist in diagnosing the severity of arthritis or injury and help plan the most appropriate surgical approach.
Discussion of surgical options: Your surgeon will explain the types of knee replacement procedures available, including full and partial replacements, and the prosthetic implant options. You’ll have the opportunity to ask questions and understand what to expect from surgery and recovery.
After knee replacement surgery, your mobility will be limited, especially in the first few weeks. Making some simple adjustments to your home before your procedure can make recovery easier, safer, and more comfortable.
- Create a safe environment
Remove potential tripping hazards such as loose rugs, electrical cords, and cluttered walkways. Consider installing handrails in high-use areas like the bathroom, and use non-slip mats or a shower chair to support safe bathing. - Organise support
Ask a friend, family member, or caregiver to assist you during the early stages of recovery. Help with cooking, cleaning, transport, and daily tasks can make a big difference while you regain independence. - Set up a recovery zone
Create a dedicated space where you can rest comfortably and keep everything you need within easy reach, such as medications, water, phone chargers, books, and remote controls. A sturdy chair with arms (not too low) will help you sit and stand more easily.
In the weeks before your knee replacement, taking steps to physically prepare can help improve your surgical experience and support a smoother recovery.
- Exercise and strengthen
If you’re able, focus on low-impact exercises that build strength around the knee joint and improve overall fitness. A stronger body can aid post-operative mobility and enhance rehabilitation outcomes. - Quit smoking
If you smoke, it’s strongly advised to stop before your operation. Smoking can interfere with wound healing and increase the risk of complications. Your care team can offer support and resources to help you quit. - Follow your preoperative plan
You may need to adjust or stop certain medications, such as blood thinners, in the lead-up to surgery. You’ll also receive specific instructions about fasting before the procedure. Following these directions closely helps reduce risks and ensures a safer surgical experience.
While preparing your body is important, taking time to mentally and emotionally prepare for knee replacement surgery can be just as valuable. Feeling informed, supported, and ready for what’s ahead can make a meaningful difference to your experience and recovery.
Understand the journey ahead
Knee replacement surgery may relieve pain and improve mobility, but recovery takes time. It’s normal to experience some discomfort, swelling, and reduced movement in the early stages. Setting realistic goals and being patient with yourself throughout the process can help you stay motivated and positive.
Plan for rehabilitation
Physiotherapy will play a key role in your recovery. You’ll need to commit to regular sessions and follow your rehabilitation plan to help restore strength, flexibility, and function in your knee. Knowing this in advance can help you mentally prepare for the effort involved.
Stay informed and ask questions
It’s natural to feel anxious before surgery. Asking questions and discussing any concerns with your orthopaedic team can help you feel more confident and reassured. Understanding your procedure, the recovery process, and what to expect day by day can reduce stress and improve your sense of control.
As your surgery day approaches, it’s completely normal to feel a mix of anticipation and nerves. Taking a few practical steps the day before can help ease anxiety and ensure everything goes smoothly.
- Pack your hospital essentials
Prepare a small overnight bag with comfortable, loose-fitting clothes, personal hygiene items, a phone charger, and any regular medications (along with a list of them). Don’t forget your Medicare card, private health insurance details (if applicable), and any hospital admission paperwork or imaging you’ve been asked to bring. - Follow pre-operative fasting instructions
You’ll be given clear instructions about when to stop eating and drinking. It’s important to follow these fasting guidelines precisely, as they are designed to reduce the risk of complications during anaesthesia. If you’re unsure or need clarification, contact your hospital or surgical team.
On the morning of your procedure, arrive at the hospital or surgical centre at the time provided to you. The medical team will be ready to support you through each step of the process.
- Final checks and pre-operative preparation
You’ll be greeted by nursing staff and guided through the admission process. The anaesthesia team will meet with you to discuss your medical history, explain the type of anaesthetic being used, and answer any last-minute questions. - Review of the surgical plan
Before entering the operating theatre, your surgical team will confirm the details of the procedure to ensure everything is aligned with your personalised surgical plan. This is your opportunity to raise any final concerns. - Comfort and support
Every effort will be made to ensure you feel calm, informed, and as comfortable as possible before surgery begins. Once you’re ready, you’ll be transferred to theatre where your knee replacement procedure will take place.
Taking the time to properly prepare for your knee replacement can make a meaningful difference to your surgical experience and recovery.
Your total knee replacement surgical procedure
A step-by-step guide to your surgery
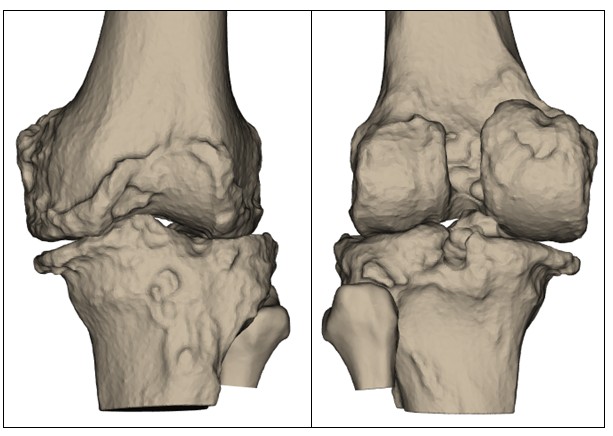
1. Planning
Using advanced imaging to guide your surgery
Before your surgery, your orthopaedic team will use detailed imaging, such as X-rays and a CT scan, to develop a personalised surgical plan. These scans provide an accurate 3D map of your knee joint, helping identify its shape, alignment, areas of cartilage loss, and how arthritis has affected joint movement. This information allows Prof. Justin Hunt or Prof. Vera Maria Sallen to plan your total knee replacement procedure with a high degree of precision. Key surgical decisions, such as where to make bone cuts, how much bone to remove, and how to position your implant, are made based on your unique anatomy.

2. Anaesthesia
Keeping you comfortable and safe during surgery
On the day of surgery, you’ll meet with the anaesthetic team to discuss the best option to keep you comfortable and safe. Most knee replacements are performed under spinal anaesthesia, which numbs the lower half of your body, though general anaesthesia may be used in some cases. Once anaesthesia has taken effect, a tourniquet is applied to the upper thigh to reduce blood flow, helping to minimise bleeding and improve visibility during the procedure. The leg is then cleaned with antiseptic and sterile drapes are positioned to maintain a clean, safe surgical environment.
3. Surgical Incision
Carefully opening the knee for accurate joint preparation
A carefully placed incision is made along the front of the knee to expose the joint. The length and position of the incision depends on your anatomy and the complexity of the procedure. Throughout this step, care is taken to minimise disruption to surrounding muscles and soft tissues, supporting a smoother recovery. Once the joint is visible, any damaged cartilage or bone is removed. Precise measurements are taken to guide the positioning and fit of your prosthetic implant, ensuring the components match your natural joint alignment as closely as possible.

4. Placement
Aligning the prosthetic components to match your natural knee
Once the joint has been prepared, the prosthetic components are positioned with a focus on restoring your natural alignment and knee movement. This step may be supported by advanced technology such as robotic-assisted systems or patient-specific instrumentation (PSI). If used, robotic or computer-assisted tools help guide the placement of the implants in real time, based on your pre-operative imaging. PSI uses 3D-printed guides tailored to your anatomy, enhancing the precision of bone cuts and implant positioning. These technologies aim to improve implant alignment, which may lead to better function and long-term outcomes. The components are secured to the bone using specialised cement or a press-fit technique, depending on your needs. Each decision is made to optimise the fit, feel, and durability of your new knee.
5. Final Adjustments
Fine-tuning alignment, motion, and joint stability before closure
Once the prosthetic components are securely in place, the surgical team performs a series of checks to fine-tune your new knee joint. This involves carefully assessing how the joint moves through its range of motion and testing for proper alignment and stability. Any necessary adjustments are made to balance the soft tissues and ensure smooth, natural movement.

6. Closure
Completing the procedure and starting the healing process
After all components are aligned and functioning as planned, the surgical site is thoroughly cleaned. The incision is closed using sutures or staples, and a sterile dressing is applied to protect the area. Your leg is gently placed into position, and the team ensures you’re stable and ready to begin recovery. From here, the focus shifts to pain management, early movement, and a structured rehabilitation plan to help you regain strength and mobility.
Recovery after total knee replacement surgery
Recovering from total knee replacement (TKA) is a vital part of your journey back to comfortable movement and everyday activity. While the surgery itself addresses the underlying joint damage, the healing process is what helps you regain strength, mobility, and confidence. At Melbourne Orthopaedic Clinic, your care team will support you through each stage of recovery, from hospital discharge to long-term rehabilitation.
After your procedure, you’ll wake up in the recovery unit, where your vital signs will be monitored as the effects of anaesthesia wear off. Discomfort is common at this stage, but you’ll be given appropriate pain relief to ensure you remain as comfortable as possible.
Most patients remain in hospital for a few days. During this time, your care team will help you begin gentle movement and physiotherapy to restore early range of motion. Walking aids such as crutches or a walker will be introduced, and you’ll be encouraged to take short, assisted walks to support circulation and prevent complications.
Pain and swelling management
Pain control is essential in the early stages to help you stay mobile and participate in rehabilitation. Your recovery plan may include:
- Prescription pain medications for the initial post-operative period – Over-the-counter medication as discomfort decreases
- Ice therapy to reduce swelling and inflammation
- Leg elevation to assist with fluid drainage
Following your tailored pain plan will help you maintain progress during your early recovery.
The initial weeks after surgery are vital for regaining strength, flexibility, and confidence in your new joint. You’ll be supported by a physiotherapist who will guide you through a tailored rehabilitation program.
Exercises will focus on improving range of motion, rebuilding muscle strength, and gradually increasing your ability to bear weight. You may continue using a walking aid during this period. To support your recovery at home:
Reduce swelling with elevation and regular use of ice packs.
Stay mobile by walking short distances regularly and avoiding long periods of inactivity.
Protect your new knee by avoiding deep bending, twisting, or kneeling until advised.
Pain will gradually lessen, and many patients find they can resume light daily activities within a few weeks.
Recovery from total knee replacement continues gradually over several months. While healing times vary from person to person, most patients experience steady improvements in pain levels, knee function, and overall mobility during this time.
As your physiotherapy progresses, the exercises will shift from basic range-of-motion activities to more advanced rehabilitation focused on improving strength, balance, and endurance. Many people begin to return to everyday tasks such as driving, recreational walking, and work, depending on their occupation and recovery progress.
- After You Leave Hospital – Once you are discharged from hospital, you’ll continue your recovery at home or in a rehabilitation facility. If you require additional pain relief after your discharge, your hospital team will typically provide a short supply of medications. After this, your General Practitioner (GP) will become your main contact for ongoing pain management. Be sure to make an appointment with your GP shortly after returning home to review your medications and ensure you have the support you need.
You’ll also receive specific instructions on how to care for your wound, manage swelling, and safely increase activity levels at home. It’s important to follow these instructions closely to reduce the risk of complications and support healing.
- Ongoing Monitoring and Support – Follow-up appointments with your orthopaedic surgeon will be scheduled to monitor your progress, assess your range of motion, and review post-operative imaging. These visits are an important part of long-term care, helping to ensure that your knee implant is functioning well and that your rehabilitation is on track.
If you notice increased pain, excessive swelling, signs of infection (such as fever, redness, or discharge from the wound), or difficulty with movement, contact your GP or orthopaedic clinic immediately.
- What to Expect Long Term – Most patients are walking confidently and have resumed low-impact activities by 3 months post-surgery. Full recovery, including return to more demanding activities or sports, can take 6 to 12 months. Remaining committed to your physiotherapy program and staying active within your limits will help you gain the most benefit from your new knee.
If needed, your surgeon or physiotherapist can advise you on safe ways to gradually return to hobbies such as swimming, golf, or cycling. Always avoid high-impact sports unless specifically cleared to do so.
Recovering from total knee replacement takes time and commitment, but the rewards can be significant. With the right support and a consistent rehabilitation plan, most people experience lasting improvements in joint function, reduced pain, and a better overall quality of life. Staying engaged in your recovery and following the guidance of your orthopaedic team will help you make steady progress toward returning to the activities you enjoy.
Risks and complications to be aware of
While total knee replacement surgery is generally safe and effective, as with any major surgical procedure, there are potential risks and complications that patients should be aware of. Understanding these risks can help you make informed decisions and prepare for your recovery.
- Infection – There is a small risk of infection around the surgical site or deeper within the joint. Preventative measures, such as sterile surgical techniques and antibiotics, are used to reduce this risk. If an infection occurs, it may require additional treatment or, in rare cases, further surgery.
- Blood clots – Blood clots (deep vein thrombosis or pulmonary embolism) can develop in the legs or lungs after surgery. To help prevent this, you may be prescribed blood-thinning medication and encouraged to move your legs soon after the procedure. Compression devices or stockings may also be used during your hospital stay.
- Implant-related issues – Although modern knee implants are designed for durability and long-term function, complications can occur. These may include loosening, wear, instability, or stiffness in the joint. In some cases, further surgery may be required if the implant becomes problematic over time.
- Nerve or blood vessel injury – Damage to nerves or blood vessels near the knee is rare but can occur. This may result in numbness, weakness, or changes in circulation. Most of these issues are temporary, but in very rare cases, they can be long-lasting.
- Ongoing pain or stiffness – While many people experience significant pain relief, some may continue to have discomfort or stiffness in the knee. This can usually be managed through physiotherapy and other supportive treatments, but in a small number of cases, persistent symptoms may remain.
- Anaesthesia risks – All surgical procedures carry risks associated with anaesthesia. These may include reactions to medications, breathing difficulties, or other complications. Your anaesthetic team will assess your medical history and work with you to determine the safest approach.
- Joint instability or dislocation – Although uncommon, the knee joint may feel unstable after surgery. This may be due to soft tissue imbalances, implant alignment, or individual anatomy. Additional physiotherapy is often helpful, but in some cases, further intervention may be needed.
Before your surgery, your orthopaedic surgeon will discuss these risks with you in more detail and provide personalised advice based on your overall health and individual needs.
Adjusting to life after a total knee replacement
A total knee replacement is a significant procedure that can offer long-term relief from chronic knee pain and restore much of your mobility and independence. While the surgical procedure and early recovery are major milestones, adjusting to life after knee replacement continues well beyond the hospital stay.
In the weeks and months after surgery, your knee will gradually become stronger and more stable. As pain levels decrease and your range of motion improves, many daily activities will become easier. However, it’s natural to feel hesitant about certain movements at first. Building confidence takes time — and the guidance of your physiotherapist will help you safely increase activity levels at a pace that suits your progress.
Regular walking, gentle strengthening exercises, and balance training can help restore your ability to perform everyday tasks such as climbing stairs, shopping, or getting in and out of a car. Over time, many people also return to low-impact recreational activities like swimming, cycling, or golf.
Depending on the nature of your work, you may be able to return within 6 to 12 weeks of surgery. Desk-based roles generally allow for a quicker return, while jobs that require prolonged standing, walking, or physical effort may take longer. Your surgeon will provide guidance based on your recovery progress and occupational needs.
You may also be able to resume driving once you have regained good strength and control in your operated leg, typically within 4 to 6 weeks. You must be confident in your ability to perform an emergency stop and safely manage the pedals before returning to the road. Check with your surgeon and your car insurance provider before driving again.
Once discharged from hospital, most patients will be sent home with a short supply of pain medication. If you require additional medication, this can be prescribed by your local GP. It’s important to attend all follow-up appointments with your orthopaedic surgeon, who will monitor your knee’s healing, implant alignment, and overall function.
You should also reach out to your GP if you experience any of the following:
Increasing or persistent pain not relieved by medication
Excessive swelling or redness around the knee
Signs of infection (e.g. fever, chills, or wound discharge)
Concerns about mobility, balance, or changes in sensation
Your GP remains an important part of your long-term care team and can liaise with your orthopaedic specialist if needed.
While a total knee replacement can significantly improve your quality of life, it’s important to keep in mind that your new knee may not feel exactly like your original joint. Some people notice occasional stiffness, mild swelling, or changes in sensation around the surgical area, especially during the first year.
By maintaining a healthy lifestyle, staying active within your limits, and following your rehabilitation plan, your knee implant can provide many years of pain relief and reliable function.
Your prosthetic knee is designed to withstand daily activity, but it’s still important to look after it. You can support its longevity by:
Avoiding high-impact sports such as running or jumping
Maintaining a healthy weight to reduce stress on the joint
Engaging in regular low-impact exercise to keep your muscles strong
Attending routine follow-up appointments as recommended
If you plan to undergo dental work or surgery in the future, always inform your dentist or doctor that you have a knee prosthesis, as antibiotics may occasionally be recommended to reduce the risk of infection.
With time, patience, and the right support, most people are able to return to a more active and fulfilling lifestyle after total knee replacement surgery. Your surgical team will continue to guide you through each stage of recovery, ensuring that your knee functions well. not just in the months ahead, but for years to come.