Total Hip Replacement (Arthroplasty)
A surgical procedure to relieve hip pain and restore function
Your hip joint supports nearly every aspect of movement, whether walking, climbing stairs, driving, or simply getting out of a chair. When hip arthritis or another hip condition causes persistent pain and stiffness, these everyday activities can become difficult and limiting.
If non-surgical treatments are no longer effective, a total hip replacement (hip arthroplasty) may be considered to help restore comfort and function. This procedure involves replacing the damaged parts of the joint with precisely selected prosthetic components that are designed to reduce pain and allow smoother movement.
Professors Justin Hunt and Vera Sallen tailor each hip replacement using advanced imaging and digital planning software. This personalised approach aims to align your new joint with your natural anatomy, supporting a smoother recovery and long-term function.
Whether your goal is to return to daily tasks without discomfort or resume a more active lifestyle, total hip replacement may help you move forward with greater ease and confidence.
Topics covered on this page include:
- What is Total Hip Replacement Surgery
- Is hip replacement right for you?
- Symptoms that may lead to hip replacement
- Choosing the best surgical approach
- Types of hip implants and how they are selected
- Benefits of total hip replacement surgery
- Personalised pre-operative planning and preparation for surgery
- What to expect during the surgical procedure
- Recovery after hip replacement: What to expect
What is Total Hip Replacement Surgery
Total hip replacement (also called total hip arthroplasty) is a surgical procedure designed to relieve pain and improve mobility in people with hip joint damage, most commonly due to arthritis.
At Melbourne Orthopaedic Clinic, Professors Justin Hunt and Vera Sallen perform this procedure using advanced surgical techniques and patient-specific planning to help restore your joint function and quality of life.
Your hip is a ball-and-socket joint that enables fluid movement and bears much of your body’s weight during walking, sitting, bending, and other daily activities. When the smooth cartilage lining the joint wears away, commonly due to osteoarthritis, injury, or other degenerative conditions, this leads to stiffness, inflammation, and pain. Over time, hip arthritis can significantly limit your ability to move comfortably or carry out everyday tasks, such as driving, walking short distances, or putting on shoes. When non-surgical treatments such as physiotherapy, medications, or injections are no longer effective, hip replacement surgery may be considered.
During a total hip replacement procedure, the damaged parts of your natural hip joint are removed and replaced with high-quality artificial components:
- The femoral head (ball) is replaced with a metal or ceramic implant
- The hip socket (acetabulum) is fitted with a new cup made of durable materials such as metal and polyethylene
- In some cases, a liner is inserted between the ball and socket to help reduce friction and wear
These components are designed to closely mimic the natural movement of your hip, restoring alignment and improving joint stability.
The primary goals of total hip replacement are to:
- Relieve chronic pain that has not improved with conservative care
- Restore mobility and movement, allowing you to return to walking and other physical activities
- Correct joint deformity or leg length differences, where applicable
- Improve your quality of life by enabling greater independence and participation in daily routines
When combined with a personalised surgical plan and structured rehabilitation, total hip replacement can offer long-lasting benefits for many patients.
Professors Hunt and Sallen focus on tailoring the procedure to each patient’s individual anatomy, health status, and lifestyle goals. Using digital imaging and 3D planning tools, they carefully select the most appropriate implant and alignment strategy to match your joint mechanics.
So, whether you are considering surgery due to advanced osteoarthritis, avascular necrosis, or other hip conditions, your care will be guided by a thoughtful and evidence-based approach designed to minimise complications and maximise outcomes.

Is Hip Replacement Right For You?
Hip replacement surgery may be considered when pain, stiffness, or reduced mobility significantly impacts your daily life and non-surgical treatments are no longer effective. The decision to proceed with surgery is highly individual, and it begins with understanding your symptoms, lifestyle goals, and the underlying cause of your hip joint damage.
You might be a candidate for total hip replacement if you are experiencing:
- Persistent pain in the groin, thigh, or buttock that limits your walking, driving, or sleep
- Difficulty with everyday tasks such as bending, standing, or climbing stairs
- Reduced hip flexibility or grinding sensations when moving
- Ineffectiveness of physiotherapy, medications, or injections in relieving symptoms
These symptoms are often caused by hip osteoarthritis, but other conditions such as rheumatoid arthritis, avascular necrosis, or previous trauma can also lead to joint deterioration requiring surgical treatment.
While many people with hip arthritis are eligible for surgery, certain medical or lifestyle factors will be considered when deciding whether now is the right time, including:
- Your age and activity level
- Your overall health and ability to recover
- Any history of joint infections, prior hip surgery, or musculoskeletal deformities
- Body weight and bone quality, which may influence surgical planning and outcomes
At Melbourne Orthopaedic Clinic, our surgeons take the time to understand your full medical history, review your imaging, and assess how your symptoms affect your life. They’ll also explore whether newer, surgical techniques like the Medacta Direct Anterior Approach (MDAA) may be appropriate in your case.
Hip replacement isn’t always the first step. If there’s still a chance of meaningful improvement through physiotherapy, medication adjustments, or joint injections, these may be recommended first. On the other hand, if surgery offers the most effective path to long-term mobility and reduced pain, our surgeons will guide you through your options, ensuring you feel confident in your next steps. Ultimately, the decision to undergo hip replacement is shared, based not only on clinical evidence, but on your personal goals, preferences, and expectations.
Professors Hunt and Sallen focus on tailoring the procedure to each patient’s individual anatomy, health status, and lifestyle goals. Using digital imaging and 3D planning tools, they carefully select the most appropriate implant and alignment strategy to match your joint mechanics.
Symptoms that May Lead to Hip Replacement
Many people live with mild hip discomfort for years before realising that the joint has progressively deteriorated. Recognising the symptoms that may indicate the need for hip replacement is the first step toward regaining your mobility and quality of life.
Common symptoms of advanced hip joint damage:
- Persistent hip or groin pain, especially during weight-bearing activities like walking or standing
- Pain that radiates to the thigh, buttock, or knee
- Stiffness that makes it difficult to bend, tie shoes, or get in and out of cars
- Reduced range of motion, making everyday movements feel restricted or awkward
- Limping or altered walking pattern to compensate for the pain
- Pain at rest or during the night, disrupting your sleep
- Reduced ability to enjoy physical activities you previously managed with ease
These symptoms often reflect conditions such as osteoarthritis, inflammatory arthritis, or post-traumatic arthritis, where the cartilage cushioning the joint has worn away, causing the bones to rub together.
When symptoms start limiting your life:
Not everyone with joint wear will need surgery but if hip pain or stiffness begins to interfere with your ability to work, care for yourself, exercise, or participate in social activities, it may be time to consider a surgical solution. At this stage, conservative treatments often provide limited relief, and total hip replacement may offer the best path forward. Professors Hunt and Sallen will assess your symptoms, review your imaging, and discuss your goals before determining whether hip replacement is the right next step.
Choosing The Best Surgical Approach
There is no single “best” way to perform a hip replacement. The most suitable surgical approach depends on your anatomy, joint condition, past medical history, and recovery goals. Professors Hunt and Sallen are highly experienced in multiple techniques and will guide you through the available options to ensure your surgery is both safe and effective.
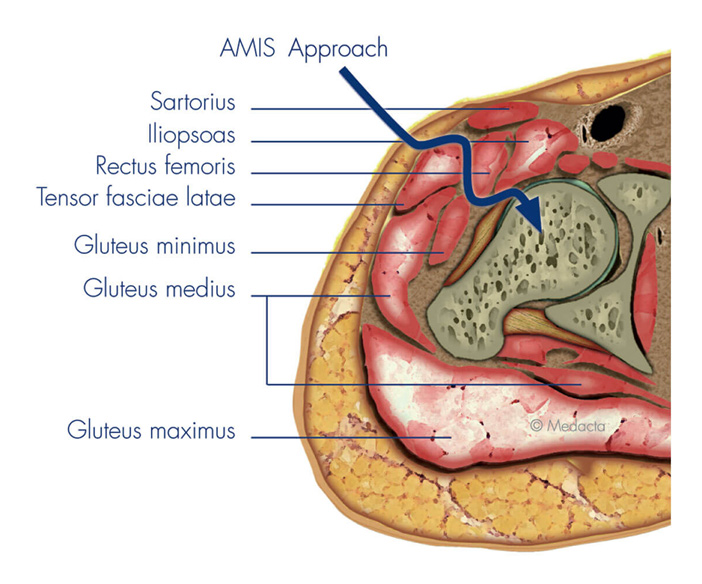
Anterior Approach (including MDAA)
The anterior approach, (AMIS/DAA) and more specifically the Medacta Direct Anterior Approach (MDAA), is a minimally invasive technique performed from the front of the hip. It avoids cutting through major muscles, which may support faster recovery, reduced post-operative restrictions, and improved early mobility. It is most appropriate for patients with standard anatomy, good bone quality, and certain body types.
Bikini Incision
For eligible patients undergoing the anterior approach, Professors Hunt and Sallen may offer a bikini incision, a cosmetically oriented skin incision placed along the natural crease of the groin. This approach may improve aesthetic outcomes, as the scar often fades more discreetly within the skin fold. While it does not change the underlying surgical technique, careful patient selection is important to ensure adequate access and a safe procedure. If a bikini incision is appropriate for you, this will be discussed during your consultation.
Posterior Approach
The posterior approach is performed through an incision at the back of the hip, it provides excellent visibility of both the acetabulum (hip socket) and the femur, making it useful in complex cases, revision surgeries, or when significant anatomical variation is present. This technique involves detaching some of the short external rotators to access the joint. These muscles are repaired at the end of the procedure, and the larger gluteal muscles are typically preserved.
Mini-Posterior Approach
In recent years, some surgeons have adopted minimally invasive modifications of the posterior approach (mini-posterior approach) to reduce soft tissue trauma. These techniques use a smaller skin incision and more targeted dissection, which may help support a smoother early recovery while still offering the benefits of traditional posterior access. The underlying surgical principles remain the same, but with greater attention to muscle preservation and early mobilisation.
Other Surgical Approach Alternatives
In selected patients, lateral or anterolateral approaches may be considered. These offer different access paths through or between the muscles around the hip and are occasionally preferred in specific anatomical situations.
Your surgeon at Melbourne Orthopaedic Clinic will consider several factors when determining the most suitable approach for your total hip replacement. These include your hip anatomy, bone quality, any previous hip surgeries or scar tissue, as well as your mobility, muscle strength, and overall health. They will also take into account your recovery goals and evaluate potential risks, such as dislocation or leg length differences, as different surgical techniques carry different risk profiles.
Types of Hip Implants and How they are Selected
Selecting the right hip implant is an important part of planning total hip replacement surgery. The materials, shape, and design of the implant influence how well the joint functions and how long it is expected to last. Your surgeon will recommend the most appropriate implant system based on factors such as your anatomy, joint condition, mobility, and activity level. This choice is guided by detailed imaging and surgical planning to ensure the implant is well-fitted and provides stable, reliable movement.
A standard total hip replacement usually involves three main components, each with a specific role in restoring joint function:
FEMORAL COMPONENT
The femoral component (stem) is the part of your hip replacement that sits inside your thigh bone (femur), providing support for the new joint. This implant choice will depend on your bone quality, the shape of your femur, and your surgical goals.

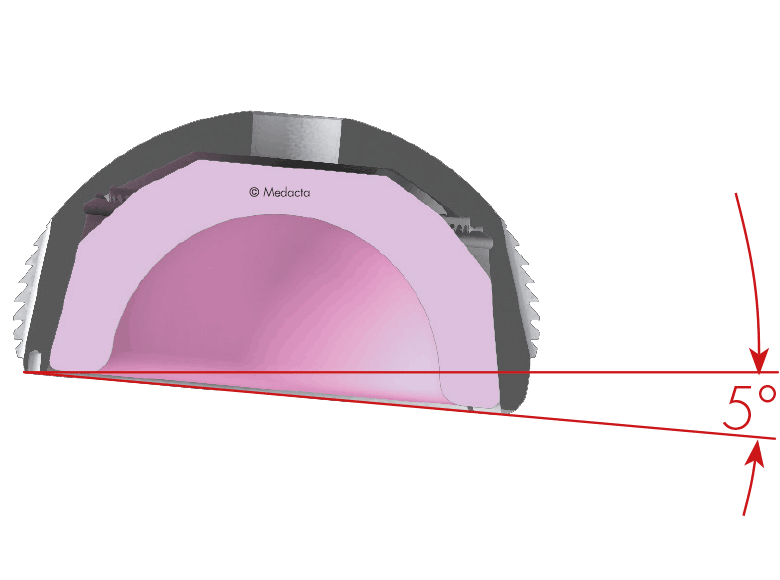
ACETABULAR COMPONENT
The acetabular component is the part of the implant that replaces the socket of your hip joint. It typically consists of a titanium shell that fits into the pelvis, and a smooth inner liner made of either ceramic or highly cross-linked polyethylene.
ARTICULAR INTERFACE
The articular interface refers to the contact point between the femoral head and the liner inside the socket. This interface is critical for smooth joint movement and the long-term performance of your hip replacement.

Potential Benefits of Total Hip Replacement Surgery
Total hip replacement can be a life-changing procedure for people living with chronic hip pain and reduced mobility. With a personalised care plan, many patients experience significant improvements in comfort, movement, and overall quality of life including:
- Pain relief and renewed comfort – One of the most immediate benefits of hip replacement is the relief of persistent pain. By removing damaged joint surfaces and replacing them with smooth, prosthetic components, the procedure aims to significantly reduce or eliminate discomfort caused by arthritis or injury.
- Improved mobility and range of motion – With the joint restored to a healthier alignment and surface, many patients find they are able to move more freely than before surgery. Everyday activities like walking, bending, or getting in and out of a car may become easier and more fluid, allowing for a return to a more active lifestyle.
- Enhanced independence and function – Reduced pain and better mobility typically lead to improved independence. Many people find they no longer need walking aids or daily assistance, which can be a major emotional and practical milestone in recovery.
- Durable outcomes that last: Modern hip implants are designed with advanced materials and engineering to last for many years. While individual outcomes vary, most patients can expect their new hip to provide long-lasting improvement, often 15 to 20 years or more, before any revision may be considered.
Personalised Pre-Operative Planning and Preparation for Surgery
To support your recovery and give you added confidence throughout your hip replacement journey, the Patient Optimized Pathway (POP) app is included as part of your care. This simple, easy-to-use digital tool provides personalised guidance at each stage – before, during, and after surgery. You’ll use this simple mobile app from the time you decide to proceed with surgery, right through to your hospital stay and rehabilitation at home. The POP app acts as your personal guide, offering timely reminders, educational resources, and practical tips tailored to your procedure. It’s designed to keep you informed, engaged, and supported at every stage. from preparation through to recovery.
In addition to the POP app, our team will guide you through key pre-operative measures to help reduce the risk of complications and support a smoother recovery.
Key preparation steps may include:
- Health and medical assessments – A thorough health review is conducted to ensure you’re fit for surgery and anaesthesia. Any medical conditions that could affect your recovery, such as high blood pressure or diabetes, will be identified and managed in advance.
- Medication review – Some medications may need to be adjusted or paused before surgery to reduce surgical risks. Your medical team will review all medications and provide clear instructions on what to continue or cease.
- Pre-surgery exercise program – A physiotherapy-led program can help strengthen the muscles around your hip and improve joint mobility. This may support a quicker return to walking and activity after your surgery.
- Education sessions – You’ll receive information about what to expect before, during, and after surgery, including how to prepare your home, use walking aids, and care for your wound. These sessions may be delivered in person or through the POP app.
To help personalise your procedure, your surgeon will use MyHip, an advanced digital planning platform that creates a 3D model of your hip based on your CT scans and X-rays. This allows for highly tailored pre-operative planning.
With MyHip, your surgical team can virtually select and position the implant to match your anatomy, assess your joint alignment, and plan for optimal leg length and offset. This level of precision aims to support better alignment, smoother joint mechanics, and a more natural-feeling hip replacement.
Where appropriate, custom 3D-printed surgical guides may be created to match your anatomy precisely. These instruments are designed to help your surgeon carry out the planned procedure in theatre with a high level of accuracy.
These guides can be used with both anterior and posterior surgical approaches and are selected based on what is most appropriate for your individual case. This technology supports surgical precision and may contribute to improved function and long-term outcomes.
During your procedure, your surgical team may use MyHip Verifier and real-time imaging tools to confirm the accurate placement of your hip components while you’re in theatre. This technology allows your surgeon to check leg length, joint offset, and component orientation against your personalised surgical plan.
By verifying key measurements during surgery, this process aims to reduce variability and support a well-balanced, well-functioning hip replacement.
All of these steps are taken to help ensure that your new joint closely matches your pre-operative plan and supports the best possible functional outcome for you.
What to Expect During the Surgical Procedure
Your journey to a successful hip replacement begins with a carefully coordinated and well-supported surgical experience. Here’s what to expect on the day of your surgery:
1. Arrival and Anaesthesia
What to expect before surgery begins
Once you’re in the operating bay, you’ll meet your anaesthesia team. They’ll review your medical history, discuss your options, and ensure you’re comfortable before surgery begins. Anaesthesia may involve general anaesthesia, where you’ll be fully asleep for the procedure, or a spinal or regional nerve block, where you remain awake but the lower half of your body is numbed. The anaesthetist will explain the benefits and risks of each option and recommend the safest and most appropriate type based on your health, preferences, and the specifics of your procedure.


2. Surgery
Surgical steps and technology used to replace your hip joint
Once the anaesthesia has taken effect, your surgeon will begin the procedure through a small incision at the front of your hip. This anterior approach works between muscle layers, helping to preserve soft tissue and potentially support faster recovery. In suitable cases, your surgeon may use a “bikini incision,” placed along a natural skin crease. The damaged joint surfaces are removed and replaced with prosthetic components . A new socket is positioned in your pelvis, and a stem with a ceramic ball is placed into your thigh bone to form your new hip joint. To guide this process, 3D planning software and customised surgical tools based on your anatomy are used. This helps with precise component placement and alignment, aiming to improve joint movement, balance leg lengths, and reduce the risk of future issues.
3. Pain Management
Local anaesthetic for post-surgical comfort
Before completing your hip replacement, your surgeon may administer a local anaesthetic around the joint to reduce pain in the hours following surgery. This can help make your initial recovery more comfortable and support early mobilisation. You may also receive medications to minimise nausea or light-headedness as the anaesthetic wears off, ensuring a smoother transition into the post-operative recovery phase.


4. Immediate Recovery
Immediate recovery in hospital
Your hip replacement surgery usually takes between one to two hours, depending on your anatomy and surgical plan. After the procedure, you’ll be moved to the recovery unit where your care team will monitor you closely as the anaesthetic wears off. Most patients spend one to two nights in hospital, with early walking encouraged, often on the same day as surgery. Early mobilisation plays an important role in reducing complications and supporting a safe and steady return to movement.
Recovery After Hip Replacement: What To Expect
Every person’s recovery is different, but there are common stages and experiences after undergoing total hip replacement surgery, particularly when performed via the direct anterior, minimally invasive approach. The following information provides a structured overview of what to expect in the early recovery phase, based on guidance from hospital physiotherapy teams and treating surgeons.
Early post-operative period
To help you feel more prepared, supported, and confident throughout your orthopaedic surgery journey, we offer access to the Patient Optimized Pathway (POP) app, a simple, easy-to-use digital tool that guides you every step of the way.
Once your surgery is confirmed, our team will register you and provide a unique access code so you can log in and get started.
DOWNLOAD ON THE APP STORE: https://apps.apple.com/us/app/patient-optimized-pathway/id1287405392
GET IT ON GOOGLE PLAY: https://play.google.com/store/apps/details?id=com.medacta.pop
Pain levels after surgery vary considerably. Some people report only mild discomfort, while others may experience more significant pain, especially during movement. Pain is typically most noticeable in the first few days and tends to improve quickly.
Your pain management plan may include:
- Spinal and/or general anaesthesia: This may provide pain relief in the first hours after surgery.
- Patient-controlled analgesia (PCA): A device allowing you to self-administer small doses of pain relief through your IV in the early hours after surgery.
- Oral medications: These may include long-acting medications like Targin® or OxyContin®, and short-acting medications such as Endone®. Anti-inflammatories like Celebrex® or Panadol® are also commonly used to reduce swelling and inflammation.
Nausea or constipation may occur as side effects of pain medications, and alternatives or additional medications can be prescribed if needed.
Swelling
It is common to experience swelling in the thigh, especially in the front (anterior compartment). This usually peaks 2–3 days after surgery and then gradually settles over the following weeks. Compression stockings and calf compressors are typically used in hospital to reduce swelling and help prevent blood clots.
Numbness or altered sensation
You may notice numbness over the side of the thigh, often due to pressure on a small skin nerve during surgery. This generally improves over time. Some people experience tingling, “electric shock” sensations, or ongoing numbness.
Bruising
Bruising around the thigh and extending to the knee is not uncommon. Blood thinning medication such as Clexane® contributes to this. Bruising usually resolves within 3–4 weeks.
Nausea and constipation
These symptoms can occur after surgery, particularly due to anaesthesia and pain medication. They are usually short-lived and can be managed with hydration, medication, and dietary adjustments.
Blood clot prevention is an important part of your recovery. You may be prescribed:
- Clexane® injections for 28 days after surgery, administered either by yourself or a family member.
- Compression stockings and calf compressors to support circulation in your legs.
- The surgical wound is typically closed with absorbable stitches and covered with a waterproof dressing.
- Keeping the wound dry is essential in the early phase to reduce infection risk.
- The wound may appear puckered due to tension from the sutures but this settles as healing progresses.
- You may also notice steri-strips on the skin and some tightness or itchiness as the wound heals.
After surgery, it’s not unusual to experience low blood pressure, especially if your usual medications have been withheld. This may cause light-headedness when standing. Maintaining hydration and slowly changing positions (from lying to sitting to standing) can help. In some cases, a low blood count (anaemia) may contribute, and a transfusion may be considered if symptoms persist.
One of the advantages of anterior minimally invasive hip replacement is that you can usually begin moving quite soon after surgery. Your physiotherapy team will help guide this process.
In hospital
You may be assisted out of bed either later the same day or the next morning, depending on the timing of your surgery and how you are feeling.
- Initial mobility: Standing with a walking frame is the first step.
- Progression: You will gradually progress to using crutches, then walking more independently as you regain strength and balance.
- Physiotherapy support: A daily program of bed and standing exercises is provided to help restore mobility and confidence.
Continue with the prescribed exercise and walking program to build your strength.
- Short, frequent walks are better than long walks in the early weeks.
- Standing exercises can be continued once bed-based exercises become easier.
- Use of walking aids: Crutches or a walking stick are recommended until you can walk confidently without limping.
- Hydrotherapy or water-based exercises may also be beneficial once your wound has healed and your surgeon gives the go-ahead.
- Sleep: You may sleep on your back or side; a pillow between your knees may improve comfort if sleeping on your side.
- Stairs: Use a step-by-step technique as guided by your physiotherapist.
- Car travel: There is no restriction on being a passenger, but you should obtain clearance from your surgeon before driving. Getting in and out of the car may be easier if the seat is reclined and slid back fully

Physiotherapy and Rehabilitation Support
Recovering well after hip replacement surgery involves more than just the operation itself. Physiotherapy and a structured rehabilitation plan play a vital role in helping you regain strength, movement, and confidence.
Your physiotherapy team is there to support and guide you through each stage of your recovery. Their goals include:
- Helping you mobilise safely from day one
- Improving strength in the hip and surrounding muscles
- Restoring a normal walking pattern
- Teaching you exercises to support joint movement
- Reducing stiffness, swelling, and risk of complications such as joint stiffness or blood clots
Your physiotherapy program begins in hospital and will often continue at home or in outpatient settings, depending on your recovery needs.
From the first day after surgery (or the same day, depending on the time of your operation), a physiotherapist will assist you to stand and walk using a frame or crutches. Daily physiotherapy sessions focus on:
- Safe movement in and out of bed
- Getting on and off chairs and the toilet
- Walking short distances
- Performing early stage exercises such as:
- Ankle pumps
- Static quads (tightening the thigh muscle)
- Gentle gluteal squeezes
- Knee bends and hip slides (bed-based)
- Standing hip flexion, abduction, and extension (with support)
Your progress is reviewed daily to ensure safe and steady improvements.
Once discharged, continuing physiotherapy is strongly recommended. You may be referred to:
- A local physiotherapist near your home
- An outpatient rehabilitation program (group or individual)
- A hydrotherapy program, once your wound has healed
Home exercises and walking form the foundation of your early rehabilitation. Your program may include:
- Standing hip and thigh strengthening exercises
- Core and balance exercises
- Gradual increase in walking distance, both indoors and outdoors
- Advice on posture and gait correction (avoiding limping)
Most patients begin with a walking frame or crutches. As your strength and balance improve, your physiotherapist will guide you in reducing support:
- Frame → 2 crutches → 1 crutch → Walking stick (as needed)
- The goal is to return to walking confidently without aids, with a normal gait
Key safety advice
- Avoid sudden twisting movements in the first few weeks
- Use supportive footwear with a non-slip sole
- Take care on stairs: follow the “good leg up, bad leg down” principle with handrail support
- Exercise within your limits: pain is not unusual, but sharp or worsening pain should be discussed with your physiotherapist or surgeon
Your physiotherapy program will be adjusted based on:
- Your age, strength, and pre-operative mobility
- Your goals (e.g. return to walking, driving, work, or sports)
- Any pre-existing conditions or joint stiffness
- Progress during the first few weeks post-operatively
In most cases, physiotherapy continues for several weeks after surgery, and many people benefit from formal guidance for 6–12 weeks depending on their recovery rate.
Pain Management and Post-Operative Care
Effective pain relief and well-managed post-operative care are critical to your recovery after hip replacement surgery. While everyone’s experience is different, the aim is to keep you as comfortable as possible while supporting safe mobilisation, wound healing, and the prevention of complications.

Pain is typically most noticeable in the first few days after surgery. Your care team will use a multimodal pain relief approach, combining different medications and techniques to manage discomfort and reduce the need for high-dose opioids.
Immediately after surgery, pain relief may include:
- Spinal anaesthesia: often provides lingering pain relief even after wearing off.
- Intravenous (IV) opioids: such as morphine, oxycodone, or a PCA (patient-controlled analgesia) device if required.
- Anti-inflammatories: such as Celebrex® or Mobic®, to reduce inflammation and associated pain.
- Regular paracetamol (Panadol®): for ongoing background pain relief.
As your recovery progresses, you will usually transition to oral medications, such as:
- Slow-release opioids: e.g. OxyContin® or Targin® for steady relief
- Short-acting opioids: e.g. Endone®, Tramal®, or Panadeine Forte® as needed
- Anti-nausea medication may be prescribed if you experience side effects from pain relief
It is normal to feel some discomfort or a sensation like a “corked thigh,” particularly when moving or walking. Pain typically improves each day.
- Swelling in the thigh is common, often peaking around 2–3 days post-surgery. It may take several weeks to settle.
- Bruising may extend down the leg and can appear dramatic, particularly if you are taking blood thinners (e.g. Clexane®). This is expected and typically fades over 3–4 weeks.
- Numbness or tingling over the outer thigh may occur due to pressure on the skin nerves during surgery. This usually resolves over time, though mild changes in sensation can persist.
Compression stockings and calf pumps are often used in hospital to help manage swelling and reduce the risk of blood clots.
After hip replacement surgery, there is a small risk of deep vein thrombosis (DVT) or pulmonary embolism. To reduce this risk, you will usually be prescribed:
- Daily Clexane® injections for 28 days (your nurse will teach you or a family member how to administer them)
- Compression stockings worn for at least 2 weeks
- Gentle leg exercises and early mobilisation
Your surgical wound will be closed using internal dissolvable sutures and covered with:
- Steri-strips to support the skin edges
- An absorbent pad and waterproof dressing to protect the site
To reduce the risk of infection:
- Keep your wound clean and dry until advised otherwise
- Avoid showering directly over the area in the first few days
- Report any signs of infection such as redness, oozing, or increasing pain
Your dressing will usually remain in place until your first follow-up or unless there are signs of loosening or fluid buildup.
Side effects such as constipation and nausea are common due to pain medications and reduced activity.
To manage these:
- Stay well hydrated
- Eat a high-fibre diet
- Use laxatives if needed (as prescribed)
- Let your team know if nausea persists so they can adjust your medications
It’s not unusual to feel light-headed or tired in the days after surgery. This can be due to:
- Anaesthetic effects
- Temporary low blood pressure
- Blood loss during surgery, especially in smaller patients
Your haemoglobin levels will be checked after surgery. In some cases, a blood transfusion may be recommended to assist recovery if you are significantly anaemic and experiencing symptoms.
You will be encouraged to stand and walk on the same day as your operation (or the day after), with support from nursing and physiotherapy staff. Weight-bearing is allowed unless otherwise instructed.
Walking aids such as a frame or crutches will be provided for support as you begin to move around safely.
Life After Hip Replacement: Returning to Daily Activities
Following your total hip replacement, regaining independence and returning to your regular activities is a gradual process that takes time, patience, and support. While each person’s recovery is unique, many patients experience a steady improvement in pain, movement, and function within the first few months after surgery.
Resuming Movement and Everyday Tasks
You’ll begin walking initially, with a walking aid within a day of surgery, guided by your physiotherapist. As your strength and confidence improve, you’ll gradually reduce your reliance on walking aids. Most people can return to light everyday activities such as dressing, bathing, and walking around the house within a few weeks.
It’s important to follow any movement precautions or activity restrictions advised by your surgeon or physiotherapist, particularly in the early recovery phase. These are designed to protect your new hip as it heals.
Driving and Transport
You may be able to return to driving around 4–6 weeks after surgery, depending on your progress, which leg was operated on, and whether you are taking pain medications. Your surgeon will assess your readiness and provide clearance before you resume driving.
Work and Hobbies
The timeframe for returning to work varies depending on the type of work you do. Sedentary or desk-based roles may be resumed within 4–6 weeks, while jobs that involve physical labour may require a longer recovery period. Hobbies like gardening, golf, or swimming can usually be reintroduced gradually under the guidance of your care team.
Sexual Activity
Most people can resume sexual activity after 4–6 weeks, once pain has settled and movement has improved. Your physiotherapist or surgeon can provide personalised advice on safe positions and precautions.
Travel and Holidays
Domestic and short-distance travel may be possible within a few weeks, but longer trips, especially by air, may increase your risk of blood clots in the early stages. It’s important to discuss any planned travel with your surgeon and consider compression stockings or blood-thinning medication if flying.
Long-Term Lifestyle
Your new hip is designed to improve your quality of life and allow you to return to many of the activities you enjoy. Low-impact exercises like walking, cycling, swimming, or Pilates are generally encouraged and beneficial for joint health. High-impact sports, running, or heavy lifting may not be recommended, as they could increase the wear on your implant.
Frequently Asked Questions About Total Hip Replacement Surgery
The anterior and posterior approaches to total hip replacement surgery are two widely used methods, each with its own advantages and considerations:
ANTERIOR APPROACH –The anterior approach (AMIS approach) to hip replacement involves accessing the hip joint from the front of the hip, rather than the side or back. This method allows me to work between the muscles without cutting through them, minimising muscle damage.
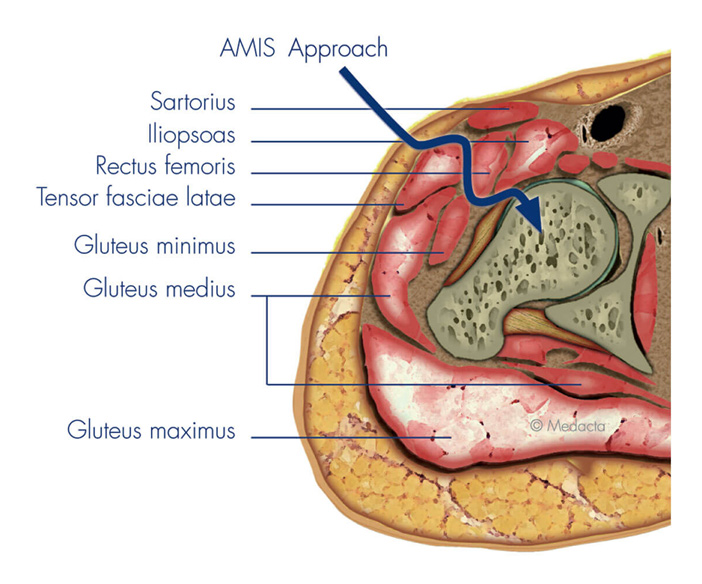
Anterior Approach Potential Advantages:
- Reduced Muscle Damage: Since the approach avoids cutting major muscles, patients often experience less post-operative pain and a quicker initial recovery.
- Faster Recovery: Many patients are able to walk sooner after surgery, sometimes within hours or the next day, due to less muscle trauma.
- Reduced Risk of Dislocation: The anterior approach may lower the risk of hip dislocation post-surgery, as the hip’s posterior structures are left intact.
- Improved Range of Motion: Patients might benefit from a more natural range of motion sooner after surgery, with fewer restrictions during the recovery period.
Anterior Approach Potential Considerations:
- The anterior approach requires specific surgical expertise and equipment. Not all surgeons are trained in this technique, making it less available in some regions.
- In some cases, the surgery might take slightly longer due to the technical precision required.
- Visibility of the hip joint might be more limited compared to the posterior approach, although advanced imaging techniques can mitigate this issue.
Anterior Approach Post-Op precautions:
NONE
Common post-operative guidelines after Anterior Hip Replacement include the following:
- You may bend your hip immediately after surgery and bear full weight when comfortable.
- Your surgeon will prescribe pain medications to keep you comfortable at home.
- Keep the incision clean and dry. You may shower once the dressings are removed unless otherwise directed by your surgeon.
- You will be given specific instructions regarding activity and rehabilitation. You will not have to follow standard hip precautions.
- Physiotherapy will be ordered to restore normal hip function and strength.
- If you are having any procedures such as dental work or any other surgery you should take antibiotics before and after to prevent infection in your new prosthesis.
- Your hip replacement may go off in a metal detector at the airport.
- Eating a healthy diet and not smoking will promote healing.
POSTERIOR APPROACH – The posterior approach accesses the hip joint from the back (posterior) of the hip. This traditional method has been the standard for many years and is widely practiced.
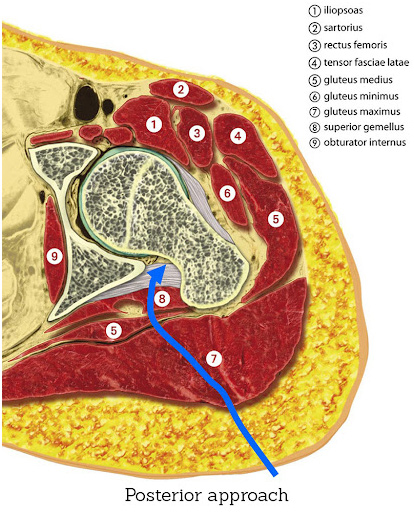
Posterior Approach Potential Advantages:
- Familiarity: Many surgeons are trained in this approach, making it widely available.
- Better Joint Visibility: The posterior approach provides excellent visibility of the hip joint, which can be beneficial in complex cases.
- Versatility: This approach can be adapted for a wide range of patients and hip conditions, offering flexibility in handling various surgical scenarios.
Posterior Approach Potential Considerations:
- Muscle Damage: The approach involves cutting through major muscles at the back of the hip, which can lead to longer initial recovery periods and greater post-operative pain.
- Risk of Dislocation: There’s a slightly higher risk of hip dislocation after surgery, necessitating more precautions during the recovery period.
- Longer Recovery: Patients may take longer to return to certain activities, with more restrictions on movement to prevent dislocation.
Posterior Approach Post-Op Precautions:
Posterior Approach Post-op precautions are very restrictive and usually include the following:
- Avoid the combined movement of bending your hip and turning in your foot.
- You should sleep with a pillow between your legs for 6 weeks.
- Avoid crossing your legs and bending your hip past a right angle.
- Avoid low chairs.
- Avoid bending over to pick things up. Grabbers are helpful as are shoehorns or slip on shoes.
- An elevated toilet seat should be used.
Most patients return to normal, low-impact activities, enjoying significant mobility improvements. Dr. Hunt will guide you through the recovery process to ensure the best outcomes.
While there may be temporary restrictions on certain movements or activities immediately after surgery, such as bending at the hip or lifting heavy objects, most patients can gradually return to their normal activities over time. Dr Hunt will provide specific guidance on activity restrictions and limitations during the recovery period.
The timing for returning to work and driving after hip replacement surgery varies widely among patients and is influenced by several factors, including the type of work you do, your overall health, and your progress during rehabilitation. Generally, most patients can expect to return to sedentary or desk-based work within 4 to 6 weeks following surgery, provided their recovery is progressing well and they have clearance from their surgeon. More physically demanding occupations may require a longer recovery period, typically ranging from 8 to 12 weeks or more.
Regarding driving, patients typically need to wait until they have regained sufficient strength, mobility, and reaction times to safely operate a vehicle. This often occurs around 4 to 6 weeks post-surgery, but it ultimately depends on individual factors and should be discussed with Dr Hunt during follow-up appointments. It’s essential to follow his guidance and any driving restrictions imposed by local regulations or insurance policies to ensure a safe return to driving.
Some patients may require assistive devices such as a walker, cane, or crutches during the initial stages of recovery to aid with mobility and balance. The Melbourne Orthopaedic healthcare team will assess your needs and provide recommendations for any necessary equipment.