Spinal Fractures
A serious injury involving a break in one or more vertebrae
Spinal fractures occur when one or more of the vertebrae in the spine crack or break. They may result from trauma such as a fall, motor vehicle accident, or sports injury, but can also occur in weakened bones due to conditions like osteoporosis.
The severity of spinal fractures varies. Some may be small, stable fractures causing mild pain, while others can be more serious, leading to spinal instability or pressure on the spinal cord and nerves. Symptoms may include localised back pain, difficulty moving, or in severe cases, neurological changes such as numbness, weakness, or loss of function.
Diagnosis and treatment depend on the location and extent of the fracture, as well as whether the spinal cord or surrounding nerves are affected.

Causes of Spinal Fractures
Spinal fractures can develop from a variety of factors that weaken or place excessive force on the vertebrae. Common causes include:
- Trauma – High-impact events such as motor vehicle accidents, falls, or sports injuries are leading causes of spinal fractures. The force of these incidents can break or displace the vertebrae, sometimes resulting in spinal instability.
- Osteoporosis – This condition weakens the bones, making them more brittle and prone to compression fractures, often from minor falls or even everyday activities.
- Degenerative changes – Long-term wear and tear on the spine can reduce bone strength and stability, increasing the risk of fractures.
- Tumours – Cancer that spreads to the spine can weaken the vertebrae, making them more likely to fracture.
- Infections – Rarely, infections in the spine can weaken bone structure and lead to fractures.
The underlying cause plays an important role in determining treatment, as managing bone health and addressing contributing conditions is essential for long-term recovery.
Symptoms of Spinal Fractures
The symptoms of a spinal fracture can vary depending on the location of the injury, the severity of the break, and whether nerves or the spinal cord are affected. Common signs and symptoms include:
- Back pain – Sudden, sharp pain at the site of the fracture, which may worsen with movement.
- Loss of mobility – Difficulty standing, walking, or bending due to pain or instability.
- Deformity or misalignment – Visible changes in posture, such as a hunched back (kyphosis) or uneven spine, particularly in compression fractures.
- Neurological symptoms – Numbness, tingling, weakness, or loss of sensation in the arms or legs if the fracture compresses the spinal nerves or cord.
- Loss of bladder or bowel control – In severe cases, fractures may cause spinal cord compression leading to changes in continence, which requires urgent medical attention.
Symptoms may appear immediately after an injury, but in cases such as osteoporosis-related compression fractures, pain can develop gradually over time.
Diagnosis of Spinal Fractures
Diagnosis begins with a medical history and physical examination. Your doctor will ask about how the injury occurred, any underlying conditions such as osteoporosis, and the type and severity of symptoms you are experiencing. A physical assessment may include checking for tenderness, spinal alignment, mobility, and neurological function.
Imaging tests
To confirm the presence and extent of a fracture, imaging is usually required:
- X-rays – Often the first test, X-rays can identify obvious fractures, changes in vertebral height, or spinal alignment issues.
- Computed tomography (CT) scan – Provides detailed cross-sectional images of the spine, helping to assess the size, shape, and exact location of the fracture.
- Magnetic resonance imaging (MRI) – Useful for assessing soft tissue, nerve involvement, and whether the spinal cord is affected. MRI can also help identify fractures caused by underlying conditions such as osteoporosis, infection, or cancer.
The combination of clinical assessment and imaging helps determine whether the fracture is stable or unstable, if nerves are involved, and what treatment approach is most appropriate.
Treatment Options for Spinal Fractures
The management of spinal fractures depends on the cause, severity, stability of the fracture, and whether the spinal cord or nerves are affected. The main goals of treatment are to relieve pain, promote healing, restore stability, and prevent further injury.
Non-surgical treatments
Stable or less severe fractures may be managed without surgery. Options include:
Pain management – Medications such as anti-inflammatories or analgesics can help relieve discomfort.
Bracing – A spinal brace may be used to support the spine, limit movement, and promote healing.
Physiotherapy – Once initial healing has occurred, a physiotherapy program can strengthen supporting muscles, improve mobility, and aid recovery.
Activity modification – Reducing strenuous activities and avoiding heavy lifting until healing has progressed.
Treatment of underlying causes – For example, addressing osteoporosis with medications or lifestyle measures to reduce the risk of future fractures.
Surgical treatments
Surgery may be considered if the fracture is unstable, causes significant pain, or places pressure on the spinal cord or nerves. Surgical options include:
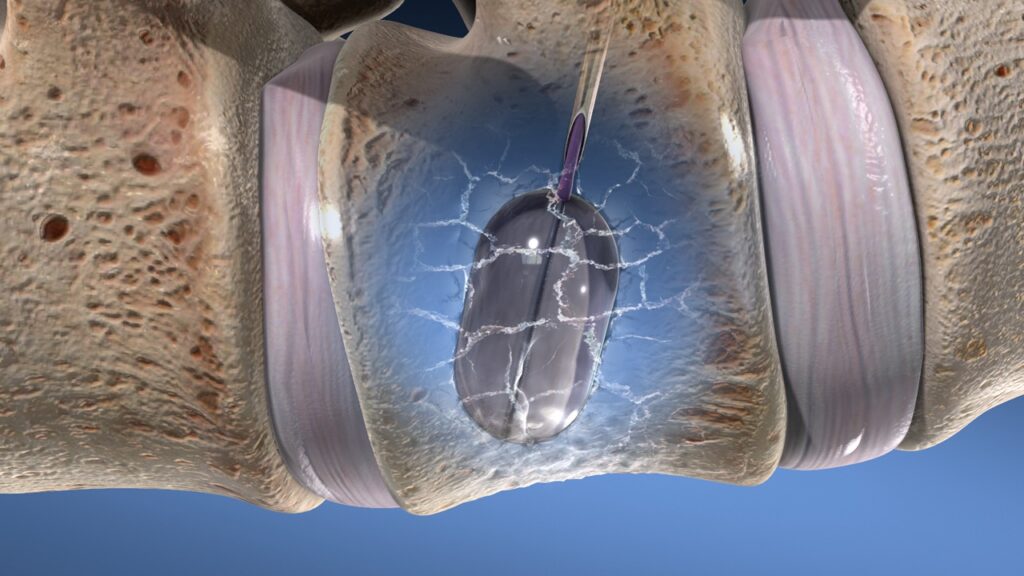
Vertebroplasty or kyphoplasty – Minimally invasive procedures where bone cement is injected into the fractured vertebra, sometimes with a balloon to restore height before cement placement.
Spinal decompression – Removal of bone or tissue pressing on the spinal cord or nerves.
Spinal fusion – Joining two or more vertebrae together with bone grafts and instrumentation (such as screws and rods) to stabilise the spine.
The choice of treatment is individual and depends on the type of fracture, overall health, and recovery goals.