Sciatica
A condition characterised by pain that radiates along the sciatic nerve
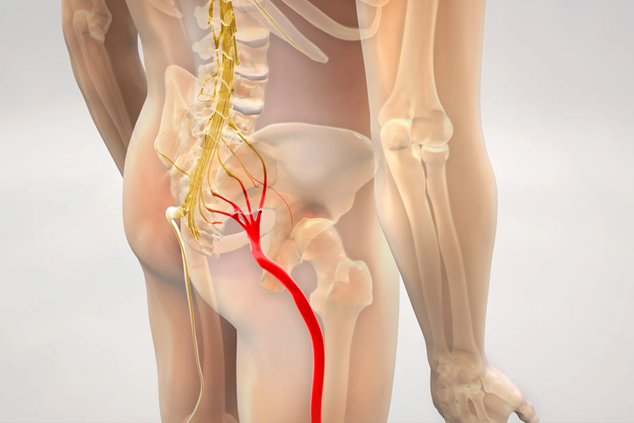
Sciatica describes pain that travels along the path of the sciatic nerve, which runs from the lower back through the hips and buttocks and down each leg. It occurs when the nerve is compressed or irritated, most commonly by conditions such as a herniated disc, spinal stenosis, or other changes in the spine.
Symptoms can range from mild discomfort to severe, sharp pain, and may be accompanied by tingling, numbness, or weakness in the affected leg. The severity and pattern of symptoms vary depending on the cause and the degree of nerve involvement.
Management of sciatica depends on the underlying cause and may include non-surgical treatments such as physiotherapy, medications, or injections. In some cases, surgery may be considered if symptoms persist or worsen.
Causes of Sciatica
Sciatica develops when the sciatic nerve is compressed, irritated, or inflamed. Several spinal conditions can contribute to this, including:
- Herniated disc – The soft inner portion of a spinal disc can bulge or rupture, pressing on the nearby nerve roots. This is one of the most common causes of sciatica.
- Spinal stenosis – Narrowing of the spinal canal can place pressure on the nerves, including the sciatic nerve roots.
- Degenerative disc disease – Wear and tear on the spinal discs can lead to instability or bone spurs that irritate the nerve.
- Spondylolisthesis – A vertebra slipping forward out of place can compress the nerve roots that form the sciatic nerve.
- Muscle spasm or inflammation – In some cases, surrounding muscles or soft tissues can irritate the sciatic nerve.
- Trauma or injury – Accidents or falls may directly damage the spine or nerve roots.
Less commonly, tumours, infections, or other spinal abnormalities may also affect the sciatic nerve.
Symptoms of Sciatica
Sciatica is characterised by pain that follows the path of the sciatic nerve, but the exact symptoms can vary depending on the severity and cause of the nerve irritation. Common features include:
- Pain – Often described as sharp, burning, or shooting pain that starts in the lower back or buttock and travels down the back of the thigh, calf, or foot. Pain usually affects only one side of the body.
- Numbness or tingling – A “pins and needles” sensation may be felt in the leg, foot, or toes.
- Weakness – Some people experience weakness in the affected leg, making it difficult to stand, walk, or lift the foot.
- Worsening with movement – Symptoms often increase with activities such as sitting for long periods, bending, coughing, or lifting.
- Relief with certain positions – Lying down, walking, or gentle stretching may sometimes reduce discomfort.
The severity of symptoms can range from mild irritation to disabling pain. In rare cases, severe sciatica may be associated with loss of bladder or bowel control, which requires urgent medical attention.
Diagnosis of Sciatica
Diagnosis begins with a medical history and physical examination. Prof. Hunt will ask about the nature of your pain, when it occurs, and what activities make it better or worse. He may also assess posture, reflexes, muscle strength, flexibility, and walking patterns to help identify nerve irritation.
Physical examination
- Straight leg raise test – Lifting the leg while lying down can reproduce sciatic pain and help identify nerve involvement.
- Neurological checks – Reflexes, muscle strength, and sensation in the legs are assessed to detect areas affected by nerve compression.
Imaging tests
Imaging is not always required for mild cases, but may be recommended if symptoms are severe, persistent, or progressive:
- X-rays – Can reveal bone spurs, alignment issues, or other structural changes.
- Magnetic resonance imaging (MRI) – Provides detailed images of discs, nerves, and soft tissues, and is the most common test for confirming the cause of sciatica.
- Computed tomography (CT) scan – May be used if MRI is not suitable.
- CT myelogram – Involves injecting contrast dye into the spinal canal before a CT scan to highlight nerve compression.
Nerve tests
In some cases, electromyography (EMG) or nerve conduction studies may be carried out to measure electrical activity in the muscles and identify which nerves are affected. These assessments help confirm the cause of sciatica and guide treatment decisions tailored to your individual needs.
Treatment Options for Sciatica
Treatment for sciatica focuses on relieving pain, reducing nerve irritation, and restoring normal function. The approach depends on the cause of the nerve compression, the severity of symptoms, and how much the condition interferes with daily activities.
Non-surgical treatments
Most people improve with non-surgical management, which may include:
- Physiotherapy – Exercise programs designed to strengthen the back and core muscles, improve flexibility, and support posture.
- Medications – Anti-inflammatory medicines (NSAIDs), muscle relaxants, or pain relievers may be used to reduce discomfort.
- Epidural steroid injections – Corticosteroid injections around the affected nerve roots may help reduce inflammation and provide temporary relief.
- Activity modification – Avoiding prolonged sitting or heavy lifting and engaging in low-impact exercise such as walking or swimming may ease symptoms.
- Heat or cold therapy – Applying heat or ice packs may help with pain management in some cases.
Surgical treatments
If symptoms persist or significantly affect quality of life despite non-surgical care, surgery may be considered. Options include:
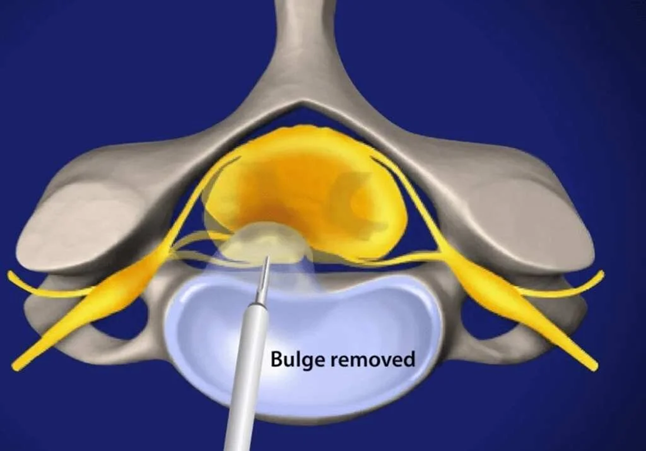
- Discectomy – Removal of part of a herniated disc that is pressing on the sciatic nerve.
- Laminectomy – Removal of part of the vertebra (lamina) to create more space and reduce pressure on the nerve.
Surgery is generally reserved for severe or persistent cases, or when sciatica is associated with neurological problems such as leg weakness or changes in bladder or bowel control.