Revision Hip Replacement Surgery
Addressing complications or wear after a previous hip replacement
If you’ve had a total hip replacement in the past and are now experiencing pain, stiffness, instability, or other complications, you may be wondering whether further surgery is needed. Revision hip replacement surgery is a specialised procedure designed to address problems with a previous hip implant and restore your comfort and mobility.
At Melbourne Orthopaedic Clinic, our surgeons use advanced imaging, surgical planning, and personalised care pathways to assess the condition of your existing implant and determine the most appropriate next steps.
Understanding when revision surgery may be needed
A hip replacement is designed to restore comfort and mobility for many years, but in some cases, problems can develop over time. Revision hip replacement may be considered when your current implant no longer performs as intended, or complications arise that affect your daily life.
Signs that may indicate a problem
Common symptoms that could suggest your hip replacement isn’t functioning properly include:
- Ongoing or worsening hip pain
- Stiffness or a reduction in movement
- A sense of instability or the hip “giving way”
- Swelling or warmth around the joint
- Difficulty walking or performing daily tasks
While these symptoms don’t always mean revision surgery is necessary, they are important to have assessed by your orthopaedic surgeon.
What imaging and investigations can reveal
If you report concerning symptoms, your surgeon may recommend diagnostic tests such as:
- X-rays – to assess implant position and signs of loosening
- CT scans – to evaluate surrounding bone and soft tissues
- Blood tests – to rule out infection
These investigations help determine whether the implant is worn, loose, dislocated, or has caused bone loss.
Situations where revision may be required
Some of the more common reasons for needing a revision hip replacement include:
- Implant wear or loosening – over time, the prosthetic parts may degrade or lose their secure fit
- Dislocation or instability – if the joint repeatedly dislocates or feels unstable
- Infection – this may occur around the implant, either early after surgery or years later
- Fracture – a break in the bone around the implant can make revision necessary
- Leg length discrepancy – when leg lengths are uneven and affecting movement
Considering your overall health and goals
Your general health and ability to recover from another surgery will also be considered. If you have conditions like diabetes, heart disease, or a history of infections, your care team may work with other specialists to optimise your health beforehand.
If conservative treatments (such as physiotherapy or pain management) are no longer effective, and investigations show that your implant is no longer performing well, revision surgery may be the most appropriate option.
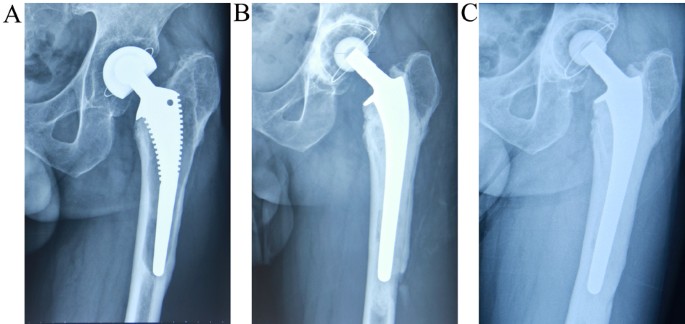
Implants and components used in revision procedures

Revision hip replacement surgery often requires specially designed implants to accommodate the unique challenges that can arise when a hip joint has already been operated on. These challenges may include bone loss, implant loosening, joint instability, or infection. Compared to primary hip replacements, revision implants are typically more robust and versatile, offering added fixation and support where standard implants may no longer be suitable.
Addressing bone loss, instability, and joint integrity
When the bone around the original implant has deteriorated or been damaged, specialised implants can help rebuild structural support. These may include:
- Longer stems to reach deeper into healthy bone and provide a more secure anchor
- Modular components that allow flexibility in tailoring the implant to your individual anatomy and bone quality
- Reinforcement devices or augments to fill bone defects and restore stability
- Dual mobility cups or constrained liners to reduce the risk of dislocation in cases of soft tissue laxity or instability
Professors Hunt and Sallen may also use bone grafts, either from your own body or a donor source, to rebuild areas where bone has been lost.
Durability and expectations
It’s important to understand that while revision implants are engineered for strength and stability, the overall durability of a revision hip replacement may be slightly lower than that of a primary hip replacement. This is due to the more complex nature of the procedure and the condition of the bone and surrounding tissues at the time of surgery.
Careful implant selection for individual needs
At Melbourne Orthopaedic Clinic, your surgeon will thoroughly assess your hip through advanced imaging and clinical evaluation before selecting the most appropriate implant components. Every revision procedure is personalised, with the goal of restoring stability, relieving pain, and supporting long-term joint function.
What to expect from the revision hip replacement procedure
Revision hip replacement is a more complex procedure than primary hip replacement and is tailored to address the specific reason your original implant is no longer functioning as intended. Here’s what you can expect at each stage of the surgical journey:
- Pre-operative planning
Before your surgery, your surgeon will carry out a comprehensive assessment to understand why your original implant has failed. This includes reviewing your medical history and ordering diagnostic imaging such as X-rays, CT scans, or MRIs. These help identify issues like loosening, wear, infection, or bone loss. Your surgical plan is then customised to your situation — including the selection of suitable implants, techniques, and contingency strategies for any expected challenges.
- Anaesthesia and surgical incision
On the day of your surgery, you’ll meet with your anaesthetist to discuss your anaesthetic plan. General or spinal anaesthesia may be recommended based on your health status and preferences. The surgical incision is usually made at or near the site of your original hip replacement. Depending on the complexity of the revision, this incision may need to be extended or modified to allow proper access to the joint.
- Removal of the original implant
The existing implant is removed with great care to avoid further damage to surrounding bone and soft tissues. If the implant has loosened, broken, or integrated tightly with bone, special tools and techniques are used to safely extract it. In cases of bone loss, bone grafts may be used to rebuild the joint structure and prepare the area for the new implant.
- Placement of the new implant
After the joint is cleaned and stabilised, the new prosthetic components are carefully positioned. Your surgeon may use cemented or uncemented fixation techniques, depending on bone quality and other individual factors. Advanced alignment and imaging tools are often used during surgery to ensure optimal positioning, joint stability, and limb length restoration.
- Closing the incision and early recovery
Once the new implant is in place, your surgeon will close the incision with sutures or staples and apply a sterile dressing. Drains may be inserted temporarily to reduce fluid build-up. Post-operative monitoring begins immediately, focusing on pain management, infection prevention, and early mobilisation with the help of the nursing and physiotherapy teams. Most patients remain in hospital for 4 to 5 days.
- Rehabilitation and long-term outcomes
Rehabilitation is a critical component of recovery after revision hip replacement. A physiotherapist will guide you through a personalised program aimed at gradually restoring strength, balance, and mobility. Because revision surgery is more demanding, recovery may take longer than your first hip replacement. Most patients can resume daily activities within six weeks, with ongoing improvements in comfort and movement over several months. By six months, many people are walking independently and experiencing meaningful improvements in quality of life.
Your recovery after revision hip replacement
Recovery from revision hip replacement surgery is often more involved than your initial hip replacement. Because the procedure is typically performed to address complications or damage to the joint, soft tissue, or bone, rehabilitation and healing may take longer and require additional support.
Immediate post-operative period
After surgery, you’ll be closely monitored in hospital for several days. During this time:
- Pain management strategies will be implemented to keep you as comfortable as possible, using a combination of medications.
- Early mobilisation is encouraged, usually within 24 hours, with support from your physiotherapy team. Gentle walking and joint movement help reduce the risk of complications such as blood clots and stiffness.
- Wound care is provided and monitored to prevent infection and support proper healing. You may have a dressing and, in some cases, surgical drains.
- Preliminary physiotherapy begins in hospital, focusing on safe movement techniques, using walking aids, and starting basic strength exercises.
Rehabilitation and physiotherapy
A tailored physiotherapy program is critical after revision surgery. Your plan may include:
- Graduated walking and weight-bearing based on your surgeon’s instructions and the type of implant used
- Targeted strengthening exercises to rebuild muscle support around the joint
- Balance and gait training to improve your walking pattern and reduce the risk of falls
- Range-of-motion work to address stiffness and help restore flexibility
This process is generally more gradual than after your first hip replacement and may continue for several months.
Returning to normal activities
Most patients begin resuming light daily activities by 6 to 8 weeks post-surgery. However:
- Driving, household tasks, and work duties may take longer depending on your job and progress.
- You’ll have regular follow-up appointments to assess healing and implant function.
- Some patients may require additional rehabilitation support or community physiotherapy depending on their baseline function and complexity of the revision.
Long-term outlook
While recovery from revision hip replacement can take longer, many patients experience significant pain relief and improved mobility once healing is complete. Your final outcome will depend on:
- The reason for your revision surgery (e.g. infection vs. mechanical wear)
- The condition of your bones and soft tissues at the time of surgery
- Your commitment to post-operative rehabilitation
Your surgeon will continue to monitor your progress over time and provide guidance to help you achieve the best possible outcome from your revision procedure.

Risks associated with revision hip replacement surgery
While revision hip replacement surgery can be an effective way to address problems with a previous hip replacement, it is a more complex procedure than primary hip replacement surgery. As with any major operation, there are potential risks that should be carefully considered and discussed as part of the informed consent process.
General Surgical Risks
As with all major orthopaedic surgery, general risks may include:
Infection
There is a risk of infection at the surgical site or around the implant. In some cases, this may require prolonged antibiotics or additional surgical treatment.Bleeding
Revision surgery may involve greater blood loss than primary hip replacement, occasionally requiring blood transfusion.Blood clots
The development of blood clots in the legs (deep vein thrombosis) or lungs (pulmonary embolism) is a recognised risk. Preventative measures are routinely used to reduce this risk.Anaesthetic risks
Complications related to anaesthesia can occur and are discussed in detail during the pre-operative assessment.
Specific Risks Related To Revision Hip Replacement Surgery
Because revision surgery involves removing and replacing existing implants, there are additional risks specific to this procedure, including:
Implant loosening or failure
While revision implants are designed to restore stability and function, there remains a risk that the revised implant may loosen or fail over time, potentially requiring further surgery.Persistent pain or stiffness
Some patients may continue to experience pain, stiffness, or functional limitations after revision surgery, particularly if there has been significant bone loss or soft tissue damage.Dislocation
The risk of hip dislocation is generally higher after revision surgery compared to primary hip replacement due to altered soft tissue tension and anatomy.Nerve or blood vessel injury
Rarely, surrounding nerves or blood vessels may be injured during surgery, which can result in weakness, numbness, or circulatory issues.Fracture of the surrounding bone
The bones around the hip joint may be more fragile, particularly if there is existing bone loss, increasing the risk of fracture during or after surgery.Reduced range of motion
Some patients may experience ongoing limitation in hip movement despite surgery, depending on pre-existing joint damage and post-operative rehabilitation.
Understanding individual risk
Not all patients experience complications, and many risks can be minimised with careful surgical planning, appropriate implant selection, and structured rehabilitation. During your consultation, your surgeon will discuss the specific risks relevant to your condition, overall health, and reason for revision surgery, allowing you to make an informed decision about treatment.