Medacta Direct Anterior Approach Total Hip Replacement (MDAA)
A personalised, muscle-sparing, total hip replacement surgical technique
At Melbourne Orthopaedic Clinic, Professors Justin Hunt and Vera Sallen offer advanced care for patients requiring total hip replacement. With extensive experience in anterior approach hip surgery, they are among the leading adopters of the Medacta Direct Anterior Approach (MDAA) in Australia.
If you’re living with persistentor, you’ve been advised that hip replacement surgery may be appropriate, understanding the different surgical techniques available is an important part of making an informed decision.
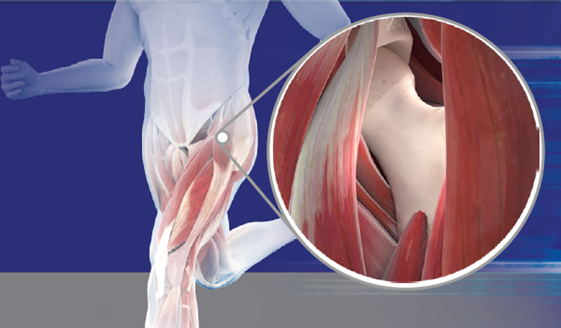
The MDAA is a refined version of the direct anterior approach. It is designed to enhance surgical precision while preserving soft tissue, which may support a smoother recovery. Unlike posterior or lateral approaches that typically involve cutting through or detaching muscle, the MDAA technique follows a natural plane between muscles and nerves at the front of the hip. This muscle-sparing approach aims to reduce tissue trauma, protect surrounding structures, and support early post-operative mobilisation.
The Medacta Direct Anterior Approach (MDAA) also incorporates specially designed instruments that allow the procedure to be performed off-table, meaning without the use of a traction table or leg positioner. This allows your surgeon greater control over the procedure, reduces equipment-related variability, and may help simplify the overall surgical process. For patients, this can mean fewer soft tissue stresses and a more consistent experience across different operating environments, while still supporting accurate implant positioning and joint stability.
Topics covered on this page:
- What is the Medacta Direct Anterior Approach (MDAA)?
- How the MDAA differs from traditional hip replacement approaches
- How MDAA is different from other anterior hip techniques
- Understanding the implants and instruments used in the MDAA technique
- Potential benefits and limitations of the MDAA technique
- Is the MDAA technique suitable for your anatomy and goals?
- Alternative surgical approaches if MDAA is not appropriate
- What to expect before, during, and after your MDAA surgery
- How Prof Hunt and Prof Sallen personalise your hip replacement
- Making a shared decision about your surgery
- Frequently Asked Questions (FAQs)
What is the Medacta Direct Anterior Approach (MDAA)?
The Medacta Direct Anterior Approach (MDAA) is an advanced technique used in total hip replacement surgery. It is based on the principles of the anterior approach, which accesses the hip joint through a natural space between muscles, avoiding the need to cut through major muscles or tendons. This muscle-sparing pathway can help reduce soft tissue trauma, potentially resulting in less pain and a faster return to movement after surgery.
What sets the MDAA apart is the refined surgical workflow developed through years of experience by leading orthopaedic surgeons including Professors Justin Hunt and Vera Sallen at Melbourne Orthopaedic Clinic. The technique is supported by a dedicated set of Medacta instruments and the use of real-time intraoperative imaging (fluoroscopy) to guide implant placement and alignment during surgery.Unlike standard anterior hip replacement techniques, the MDAA is not just a variation, it is a comprehensive, step-by-step protocol that aims to optimise:
- Protection of surrounding soft tissues and nerves
- Restoration of leg length and joint stability
- Precise implant positioning using live X-ray guidance
- Consistency in surgical exposure across different patient anatomies
The MDAA may be particularly suited to patients who are active, wish to maintain muscle function, or are seeking a swift return to work or daily activities. As with all surgical techniques, however, it is not appropriate for everyone. During your consultation, Prof. Hunt or Prof. Sallen will assess your anatomy, health, and goals to determine whether the MDAA is the most suitable approach for your hip replacement.
How the MDAA differs from traditional hip replacement approaches
The Medacta Direct Anterior Approach (MDAA) differs from traditional hip replacement techniques in several important ways. These differences relate to how the joint is accessed, how tissues are preserved, and how the implant is positioned during surgery. Understanding these distinctions can help you make a more informed decision about your treatment options.

While long-term outcomes for traditional and anterior approaches are generally similar, patients undergoing the MDAA may experience a quicker initial recovery. This is especially important for those who wish to return to work, exercise, or everyday activities as soon as possible.
Traditional hip replacement techniques, such as the posterior or lateral approaches, often involve cutting or detaching muscles and tendons around the hip joint, particularly the gluteal muscles or hip abductors, which are important for stability and walking.In contrast, the MDAA uses a natural intermuscular and internervous plane at the front of the hip. This means the surgeon can access the joint without cutting through major muscles or nerves, helping to protect soft tissue and preserve function. This may support a smoother recovery and earlier return to mobility.
A key feature of the MDAA technique is the routine use of intraoperative fluoroscopy (live X-ray guidance). This imaging allows the surgeon to continuously monitor the position of the implant, leg length, and overall hip alignment as the surgery progresses.
In many traditional techniques, such imaging is either not used or used only selectively. With the MDAA, real-time imaging helps ensure accurate implant positioning, which may reduce the risk of leg length discrepancy, dislocation, or uneven wear of the joint over time.
The MDAA is supported by a dedicated set of instruments designed to enhance the anterior surgical workflow. These tools assist in accessing and preparing the femur and acetabulum (hip socket) even in patients with more complex anatomies.Prof. Hunt and Prof. Sallen follow a clearly defined and reproducible sequence of steps, refined through extensive experience with anterior approach techniques. This structure supports consistent results and may help reduce intraoperative risks.
By avoiding major muscle disruption and using smaller incisions, the MDAA may lead to:
- Less post-operative pain
- Faster return to walking
- Shorter hospital stays
- Reduced reliance on walking aids
How MDAA is different from other anterior hip techniques
If you’ve been researching hip replacement options, you may have come across terms such as the direct anterior approach or AMIS (Anterior Minimally Invasive Surgery). These well-established techniques allow the surgeon to access the hip joint from the front of the body, rather than from the side (lateral) or back (posterior). This muscle-sparing pathway is designed to minimise disruption to surrounding tissues, which may support a faster recovery.
At Melbourne Orthopaedic Clinic, Professors Justin Hunt and Vera Sallen have helped develop a refined evolution of this technique known as the Medacta Direct Anterior Approach (MDAA). While it shares the same fundamental access pathway as other anterior techniques, the MDAA introduces important innovations that set it apart.
- Tailored surgical refinements for better visibility and control
The MDAA builds on the standard anterior approach by refining the method used to expose the femur (thighbone). This enhanced exposure improves the surgeon’s ability to visualise the joint and accurately position the implant, particularly in more complex anatomies. These refinements may reduce the risk of implant misalignment, leg length differences, or instability after surgery.
- More consistent results across a range of patients
One of the technical challenges of anterior hip replacement is achieving reliable femoral access in all patients, especially those with altered anatomy or advanced joint disease. The MDAA addresses this through subtle, evidence-based adjustments in soft tissue handling, surgical angles, and instrumentation. These modifications are designed to make the operation more predictable and reproducible, even in challenging cases.
- Experience-led innovation unique to this team
While techniques such as AMIS are widely used internationally, the MDAA has been developed and refined by Prof. Hunt and Prof. Sallen through more than a decade of experience in anterior hip surgery. Their contributions to surgical education, technique development, and instrument design have helped shape how anterior hip replacement is practised in Australia.
The MDAA integrates Medacta’s purpose-designed technologies. including specialised instruments and planning tools but remains independent of traction table systems. This off-table technique may offer greater flexibility while maintaining precision.
- Preserving the benefits of anterior access
Like other anterior techniques, the MDAA avoids cutting through key muscles around the hip. It uses the same natural interval between muscle groups to access the joint, supporting preservation of strength, balance, and mobility in the post-operative period.
In summary, the MDAA is not a brand-new surgical approach, but rather a carefully developed evolution of anterior hip replacement that combines minimally invasive principles with surgeon-led refinements for greater consistency and control. It reflects a commitment to patient-centred outcomes and high-quality care.
Potential Benefits and Limitations of the MDAA technique
As with any surgical technique, the Medacta Direct Anterior Approach (MDAA) offers a range of potential benefits, but it also comes with considerations that may make it unsuitable for some individuals. Professors Justin Hunt and Vera Sallen will carefully assess your anatomy, health history, lifestyle, and goals when recommending the most appropriate surgical approach for your hip replacement.
POTENTIAL BENEFITS OF THE MDAA
The MDAA follows a natural anatomical interval between muscle groups at the front of the hip joint. This allows the surgeon to access the joint without cutting through major muscles or tendons. This may contribute to:
- Reduced post-operative discomfort
- Faster early functional recovery
- Earlier return to walking, driving, and daily activities
The MDAA allows direct visualisation of key pelvic and femoral landmarks during surgery, supported by real-time imaging. This may assist with:
- Accurate implant placement
- Restoration of leg length
- Reduced risk of dislocation
- Improved long-term joint function
Prof Hunt and Prof Sallen use advanced 3D pre-operative planning tools and intraoperative fluoroscopy to support optimal alignment and biomechanics.
In many patients, the anterior approach allows for a smaller incision over the front of the hip. While actual incision length depends on body shape and surgical complexity, a smaller incision may:
- Lead to less visible scarring
- Support faster wound healing in some cases
By preserving key muscles around the hip, many patients are able to mobilise with support shortly after surgery. This can contribute to:
- Reduced time in hospital
- Faster return to personal care and mobility
- Earlier participation in rehabilitation
LIMITATIONS AND CONSIDERATIONS
The MDAA is a technically demanding procedure and may not be appropriate for all patients. For example:
- Individuals with a high body mass index (BMI) or dense muscle bulk
- Patients with abnormal hip anatomy or significant bone deformities
- Complex revision procedures
In these situations, another surgical approach may provide better access or safety. This will be discussed with you during pre-operative planning.
Because the surgical incision is close to the lateral femoral cutaneous nerve (LFCN), some patients may experience:
- Temporary numbness
- Tingling or altered sensation on the outer thigh
These symptoms are usually mild and improve with time, though in rare cases, they may persist.
The MDAA technique should only be performed by surgeons who are well-trained and experienced in its methods and instrumentation. Prof Hunt and Prof Sallen have contributed to the development and teaching of this technique and are recognised as national leaders in its safe application.
While the MDAA does not use a traction table, it does require specialised surgical instruments and access to intraoperative imaging (fluoroscopy). Not all facilities may be equipped for this approach. Surgeon expertise and hospital capabilities remain key factors in ensuring safe and effective outcomes.

Understanding the implants and instruments used in the MDAA surgical technique
Total hip replacement involves removing the damaged surfaces of the hip joint and replacing them with artificial components (prostheses). With the Medacta Direct Anterior Approach (MDAA), specific implants and instruments are selected to support muscle preservation, precision implant placement, and patient-specific alignment.At Melbourne Orthopaedic Clinic, Professors Justin Hunt and Vera Sallen tailor every hip replacement using advanced digital planning and surgical tools to match the procedure to your unique anatomy.
Hip implant components used in the MDAA
The MDAA technique is compatible with a range of modern, high-performance implants. Your surgeon will recommend the most suitable option based on your age, lifestyle, activity level, bone quality, and hip anatomy.
Typical implant components include:
ACETABULAR CUP
- Replaces the socket of your natural hip joint
- Usually made from titanium
- May include a durable plastic liner or ceramic insert
- Often secured by press-fit and sometimes screws for added stability

FEMORAL STEM
- Inserted into the thigh bone (femur) to support the new ball (femoral head)
- Typically made of titanium and designed to allow bone to grow into it (biological fixation)
- Selected for shape, size, and compatibility with your bone structure

FEMORAL HEAD (BALL)
- Articulates inside the acetabular cup
- Common materials include ceramic or metal
- Chosen based on wear performance and compatibility with the cup
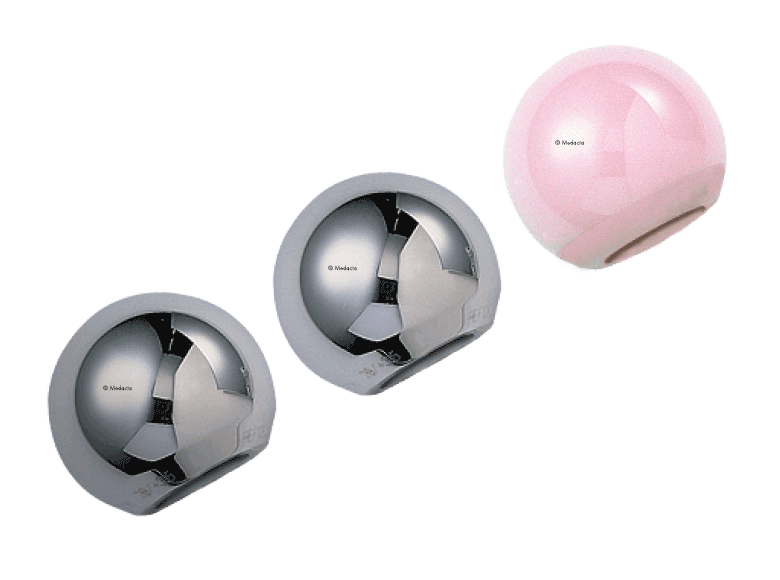
IMPLANT BEARING COMBINATIONS
Common bearing combinations:
- Ceramic-on-polyethylene: Popular for active adults due to its balance of durability and low wear
- Ceramic-on-ceramic: May be used in younger, highly active patients
- Dual mobility: Offers additional stability and may be used in select patients at higher risk of dislocation

Instrumentation & technology:
MDAA SURGICAL INSTRUMENTS
The MDAA is performed using a purpose-designed set of instruments created to assist with the anterior approach while protecting surrounding muscles and tissues. These include:
Used to gently move muscles aside without cutting them.
These help prepare the femur through a minimal incision.
Used to accommodate the unique angle of approach from the front of the hip.
These assist in accurate orientation of implants relative to your anatomy.
Temporarily inserted during surgery to assess leg length, joint stability, and range of motion before final implants are secured

Unlike some other anterior approaches, the MDAA does not require a traction table. Instead, it uses a refined exposure technique and specialised instruments to enable femoral access and implant placement while maintaining soft tissue integrity.
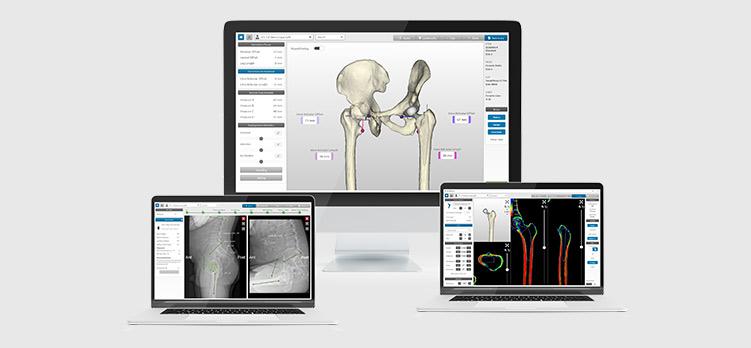
DIGITAL SURGICAL PLANNING WITH MYHIP
Prof Hunt and Prof Sallen frequently use MyHip, a 3D planning system that creates a digital model of your hip joint based on pre-operative imaging. This supports:
- Accurate sizing and selection of implants
- Detailed planning of implant position and angles
- Anticipation of any anatomical challenges before surgery
This level of planning is particularly important in minimally invasive techniques like the MDAA, where visibility is more limited, but precision is essential.
What to expect before, during, and after your MDAA surgery
If you’re preparing for a total hip replacement using the Medacta Direct Anterior Approach (MDAA), it’s completely normal to have questions. Understanding each stage of the journey, from your initial appointments to your recovery at home can help you feel more confident and in control. This guide outlines what to expect when having your surgery with Prof Justin Hunt or Prof Vera Sallen at Melbourne Orthopaedic Clinic.
Your care begins well before the day of surgery with a detailed evaluation and personalised planning.
- Clinical and medical assessment
- Review of your general health and medical history
- Evaluation of your current medications
- Identification of any risks or medical issues to address before surgery
- Hip imaging and 3D planning
- Specialised X-rays and CT scans are used to create a 3D model of your hip
- Your surgeon uses MyHip™ software to plan the ideal implant size and position for your anatomy
- Education and discussion
- You’ll learn about the MDAA technique and why it may be suitable for your case
- Your surgeon will explain the benefits, risks, and expected outcomes
- You’ll have an opportunity to ask questions and discuss your goals for recovery
- Preparation steps
You’ll receive instructions on:
- When to stop certain medications (like blood thinners)
- How long to fast before surgery
- What to bring to hospital
- Planning support for your return home
- The procedure is performed under spinal or general anaesthetic
- You’ll lie on your back in a supported position (no traction table required)
- A small incision is made at the front of your hip
- Muscles are gently separated (not cut)to access the joint
- Damaged joint surfaces are removed and replaced with the planned prosthetic components
- Intraoperative assessments check leg length, joint stability, and range of motion before closing the incision
This approach is designed to preserve important muscles, which may support faster healing and a more natural movement pattern post-op.
Most patients stay in hospital for 1 to 3 days, depending on recovery progress.
You can expect:
- Pain relief managed with medications and ice packs
- Physiotherapy beginning within 24 hours to assist with walking and mobility
- Wound care instructions and guidance on medications and exercises
- Support to help you move safely and regain independence before discharge
Prof Hunt and Prof Sallen will liaise with your nursing and rehab team to ensure a smooth transition to home.
Most patients are able to return home with a walker or walking aid, gradually regaining independence.
What to expect:
- Walking with or without support within days to weeks
- Minimal movement restrictions compared to traditional hip surgery (unless otherwise advised)
- Daily home exercises to improve strength, flexibility, and gait
- Driving may resume within 2 to 4 weeks, once you’re safe and confident
You’ll attend follow-up appointments with your surgeon to monitor healing and assess progress.
Long-Term Recovery: Returning to Life
In the weeks and months following your hip replacement, you can expect continued improvement in function, mobility, and comfort.
- Most people return to normal daily activities by 6 to 12 weeks
- You can gradually reintroduce low-impact activities such as walking, swimming, and cycling
- Higher-impact sports may be discussed on a case-by-case basis
- Ongoing reviews may be scheduled to monitor your implant and joint health over time

How Prof Hunt and Prof Sallen personalise your treatment plan
At Melbourne Orthopaedic Clinic, no two hip replacements are treated the same. Prof Justin Hunt and Prof Vera Sallen are nationally recognised orthopaedic surgeons who have helped refine the Medacta Direct Anterior Approach (MDAA) to make it safer, more accurate, and adaptable to a broad range of patients. Their approach is grounded in tailored care, ensuring every step of your journey reflects your unique anatomy, goals, and lifestyle.
Your personalised care starts with an in-depth evaluation to understand your current health, hip condition, and functional expectations.
This includes:
- A detailed physical examination and mobility assessment
- Review of your X-rays, CT scans, or MRIs
- Discussion of your medical history, lifestyle, and any past surgeries
- Analysis of walking pattern, strength, and joint flexibility
This comprehensive evaluation helps determine whether the MDAA is suitable for your individual case and sets the foundation for your treatment plan.
Prof Hunt and Prof Sallen use cutting-edge 3D surgical planning software (MyHip) to develop a strategy customised to your hip anatomy.
Using these digital tools, they can:
- Virtually map your bone structure and joint mechanics
- Select the most appropriate implant size and positioning
- Plan leg length restoration and joint alignment with precision
- Anticipate any surgical challenges based on your unique features
This precise level of planning is especially important for the MDAA approach, where component positioning and preservation of soft tissue are critical.
You’ll be actively involved in your care every step of the way. Prof Hunt and Prof Sallen take time to explain your options, including:
- Whether the MDAA is the best approach for your needs
- What alternatives may exist if the anatomy is not suitable
- What to expect during surgery, hospital stay, and recovery
- Risks, benefits, and likely outcomes tailored to your health and activity level
You’re encouraged to ask questions and share your goals, whether they include returning to work sooner, playing sport again, or simply walking without pain. These priorities are used to guide your care decisions.
After surgery, your recovery pathway is tailored to your needs, home situation, and pre-operative mobility.
This may include:
- Specialised physiotherapy exercises for anterior hip recovery
- Supportive walking aids adjusted to your strength and confidence
- A staged return to activity based on your progress
- Regular follow-up with Prof Hunt or Prof Sallen to monitor your healing
By aligning the surgical technique with your specific rehabilitation needs, the goal is to help you return to daily life with greater confidence and reduced risk of complications.
Is the MDAA technique suitable for your anatomy and goals?
Is the MDAA technique suitable for your anatomy and goals?
Every patient’s body, lifestyle, and goals are unique, and not every surgical approach is right for everyone. At Melbourne Orthopaedic Clinic, our surgeons take time to thoroughly assess whether the Medacta Direct Anterior Approach (MDAA) is the most appropriate option for your hip replacement.
The MDAA is designed to take advantage of the natural muscle planes at the front of the hip. It may be suitable if you have:
- Standard or mildly altered bone structure, without major deformities in the pelvis or femur
- Good bone quality, allowing for stable fixation of implants
- Healthy soft tissues, including intact muscles and tendons around the joint
Your imaging, X-rays, CT scans, or 3D reconstructions will be carefully reviewed by your surgeon to assess whether your anatomy is compatible with the anterior approach. Digital surgical planning using MyHip software allows Prof Hunt and Prof Sallen to map the implant positions before surgery begins.
While the MDAA can be used in many patients, certain factors may make it more technically complex, including:
- A higher body mass index (BMI), which may limit access and visualisation
- Previous hip surgery or significant scar tissue, which may alter the muscle planes
- Spinal or pelvic deformities, which can change joint orientation and leg length balance
If these or other challenges are present, your surgeon may recommend an alternative surgical technique to ensure safety and long-term success.
The MDAA may be well-suited to patients who:
- Want to return to walking, driving, or work as soon as possible
- Prefer minimal post-operative movement restrictions
- Are focused on preserving muscle function and joint stability
- Value a smaller or more cosmetically discreet incision
During your consultation, Prof Hunt or Prof Sallen will discuss how your goals align with the advantages of the MDAA and what recovery might look like for you.
While this overview can help you understand the general considerations, the final decision will always be made in close consultation with your surgeon. During your appointment, they will:
- Review your imaging and health history
- Discuss risks and benefits of the MDAA and other surgical options
- Talk through your expectations and recovery preferences
The ultimate aim is to offer a safe, effective, and personalised treatment plan that restores your mobility and improves your quality of life.

Alternative surgical approaches if MDAA is not appropriate
While the Medacta Direct Anterior Approach (MDAA) offers several benefits, it is not suitable for every patient. Factors such as your individual anatomy, body composition, history of prior hip surgery, or the complexity of your joint condition may lead your surgeon to recommend an alternative surgical technique. Below is an overview of other commonly used total hip replacement approaches. Each has unique features and may be better suited to specific clinical situations.
The posterior approach is the most widely performed hip replacement technique globally and remains an excellent option in many cases.
Key features:
- Incision is made at the back of the hip
- The gluteus maximus muscle is split, and short external rotators are detached
- Provides excellent visibility and access to both the acetabulum (socket) and femur
- Often preferred in revision surgery or complex anatomical cases
Considerations:
- Slightly higher early risk of posterior dislocation
- Patients may be advised to follow movement precautions (e.g. avoiding bending, twisting, or crossing the legs) for 6–8 weeks
- Muscle healing and return to full activity may take longer than with anterior approaches
The direct lateral approach involves an incision over the outer side of the hip and provides access by splitting the abductor muscles.
Key features:
- Often used in patients with complex deformities or poor bone quality
- Allows for stable implant positioning and reduced dislocation risk compared to the posterior approach
Considerations:
- May cause temporary or persistent weakness in the abductor muscles, which help stabilise the hip during walking
- Some patients experience a mild limp during early recovery, particularly if abductor strength is slow to return
The anterolateral approach is a variation of anterior access, with the incision made slightly to the side of the hip. It avoids the posterior structures while offering an alternative to midline anterior entry.
Key features:
- Accesses the joint through the space between the gluteus medius and tensor fascia lata muscles
- May be beneficial in patients where midline anterior access is limited by anatomical factors
Considerations:
- Like the direct lateral approach, it may affect the abductor muscles
- Less commonly used but remains a valuable option in select cases
During your consultation at Melbourne Orthopaedic Clinic, Prof Hunt or Prof Sallen will:
- Conduct a comprehensive review of your imaging and hip anatomy
- Discuss your lifestyle goals, medical history, and any previous surgeries
- Consider factors such as bone quality, mobility, muscle strength, and body habitus
Whether the MDAA or another technique is selected, their goal is always the same: to recommend the safest and most effective surgical approach to restore your hip function and support a long-term, successful outcome.
Making a shared decision about your surgery
Choosing to undergo hip replacement surgery is a significant decision, and at Melbourne Orthopaedic Clinic, Prof Justin Hunt and Prof Vera Sallen are committed to making it a collaborative one. Rather than a one-size-fits-all recommendation, your surgical plan is developed through an open, respectful discussion of your personal goals, medical history, lifestyle, and imaging results.
The goal is to ensure that you feel informed, comfortable, and supported in making the decision that best suits your life and future wellbeing.
Frequently Asked Questions (FAQs)
The Medacta Direct Anterior Approach (MDAA) is a modern refinement of the traditional anterior approach to total hip replacement. Developed and used by Professors Hunt and Sallen, the MDAA allows for improved access to the femur while preserving muscles around the hip. It is a minimally invasive, muscle-sparing technique that supports accurate implant positioning and may help facilitate a smoother early recovery.
While the MDAA is based on the direct anterior approach, it incorporates surgical refinements that enhance visibility and consistency, especially when accessing the femur. This can be particularly beneficial in patients with more complex anatomy or advanced joint degeneration. The technique maintains muscle preservation but offers greater control and reproducibility than standard anterior methods. Importantly, the MDAA is performed off-table, without requiring a traction table, allowing for greater intraoperative flexibility and improved patient positioning.
Not in every case. While many patients are suitable candidates for anterior hip replacement, your individual anatomy, bone quality, body type, and history of previous surgery will be carefully assessed. During your consultation, Prof Hunt or Prof Sallen will explain whether the MDAA or another approach is safest and most appropriate for you.
Implants used in MDAA procedures are selected to match your anatomy, lifestyle, and activity goals. Prof Hunt and Prof Sallen use prostheses that are compatible with minimally invasive anterior access and support patient-specific planning. The choice of implant is based on detailed imaging and 3D planning prior to your surgery.
Implants used in MDAA procedures are selected to match your anatomy, lifestyle, and activity goals. Prof Hunt and Prof Sallen use prostheses that are compatible with minimally invasive anterior access and support patient-specific planning. The choice of implant is based on detailed imaging and 3D planning prior to your surgery.
Hip replacement using the MDAA technique is usually performed under spinal or general anaesthesia, depending on your health status and the recommendation of your anaesthetist. Your pain relief will be carefully managed before, during, and after surgery to promote early mobility and comfort.
Yes. All hip replacements involve a surgical incision. With the MDAA, the incision is typically located at the front of the hip and is often shorter than incisions used in other approaches. Scarring varies between individuals, but most patients find that the scar fades over time.
If your anatomy or medical history means the MDAA is not ideal, Prof Hunt or Prof Sallen will recommend another surgical approach. Both are highly experienced in a range of hip replacement techniques and will guide you through your options to ensure you feel informed and confident in your care plan.