Carpal Tunnel Syndrome
A condition resulting in pain, numbness, and tingling in the hand and wrist
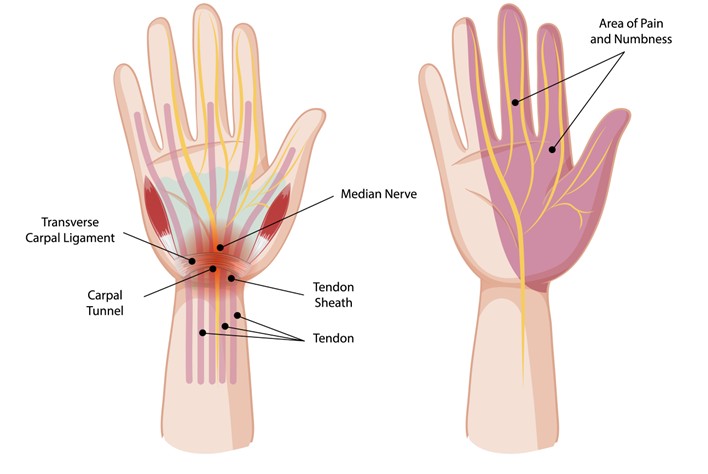
Carpal tunnel syndrome (CTS) is a condition that occurs when the median nerve, which runs from the forearm into the hand, becomes compressed within the carpal tunnel, a narrow passageway in the wrist. This compression can lead to pain, numbness, and tingling, primarily in the thumb, index, and middle fingers. Carpal tunnel syndrome is common among individuals who perform repetitive hand movements or experience prolonged wrist strain. Prof. Vera Sallen specialises in diagnosing and treating carpal tunnel syndrome to restore hand function and alleviate discomfort.
Causes of Carpal Tunnel Syndrome
Several factors can contribute to the development of carpal tunnel syndrome, including:
- Repetitive Motion: Frequent and prolonged activities involving the hand and wrist, such as typing or manual labour, can strain the tendons and cause swelling in the carpal tunnel.
- Underlying Medical Conditions: Conditions like diabetes, rheumatoid arthritis, and thyroid disorders can increase the risk of carpal tunnel syndrome due to associated inflammation or nerve compression.
- Wrist Anatomy: Individuals with a smaller carpal tunnel may be more prone to nerve compression and symptoms of carpal tunnel syndrome.
- Injury or Trauma: A wrist fracture or other trauma to the wrist can lead to swelling and increase the likelihood of median nerve compression.
Symptoms of Carpal Tunnel Syndrome
Carpal tunnel syndrome presents with a range of symptoms that may vary in intensity, including:
- Numbness and Tingling: A common symptom is a tingling or numb sensation in the thumb, index, and middle fingers, often described as “pins and needles.”
- Hand Weakness: Reduced grip strength and difficulty holding objects can occur as the condition progresses.
- Pain: Many individuals experience pain in the hand, wrist, or forearm, which may worsen at night or with prolonged use.
- Reduced Dexterity: Fine motor skills may become impaired, affecting tasks that require precise hand movements.
Diagnosis of Carpal Tunnel Syndrome
Initial consultation and medical history
Diagnosing carpal tunnel syndrome begins with a detailed discussion about your symptoms and medical history. Prof Sallen will ask about the type of discomfort you are experiencing, when it occurs, and whether certain activities make it worse. Information about your work, hobbies, and any underlying health conditions such as diabetes, thyroid disease, or arthritis is also important in building a clear picture.
Physical examination
A clinical examination is used to look for signs of nerve compression in the wrist. This may include:
- Testing sensation in your fingers
- Assessing grip and pinch strength
- Looking for muscle wasting at the base of the thumb
- Special manoeuvres such as Phalen’s test or Tinel’s sign, which may reproduce symptoms like tingling or numbness.
Nerve conduction studies and electromyography
If further information is needed, Prof Sallen may arrange for specialised tests.
- Nerve conduction studies measure how well the median nerve is transmitting signals through the carpal tunnel. A slowing of the signal can indicate compression.
- Electromyography (EMG) assesses the electrical activity of muscles supplied by the median nerve, helping to determine the severity of the condition.
Imaging
Ultrasound or MRI scans are not always necessary but may be recommended in certain cases, particularly if there is suspicion of another cause for your symptoms, such as arthritis or a wrist injury.
Establishing a diagnosis
The final diagnosis of carpal tunnel syndrome is made by combining your history, examination findings, and test results. This thorough process helps to distinguish carpal tunnel syndrome from other conditions that can cause hand or wrist pain, such as tendonitis, cervical spine problems, or peripheral neuropathy.
During your consultation, Prof Sallen will explain the results in detail and outline the most appropriate next steps for your care based on the severity of your condition and your personal circumstances.
Treatment options for Carpal Tunnel Syndrome
Treatment for carpal tunnel syndrome focuses on relieving symptoms and preventing further nerve damage. At Melbourne Orthopaedic Clinic, we offer a range of treatment options tailored to individual needs.
Non-surgical management
In many cases, symptoms of carpal tunnel syndrome can be managed without surgery, especially in the early stages. Non-surgical treatments may include:
- Activity modification – Reducing or changing activities that aggravate symptoms, such as repetitive wrist movements, may help relieve pressure on the median nerve.
- Wrist splints – Wearing a splint at night or during certain activities can keep the wrist in a neutral position and may reduce numbness and tingling.
- Medications – Non-steroidal anti-inflammatory medicines (NSAIDs) may ease pain and inflammation.
- Corticosteroid injections – In selected cases, a steroid injection into the carpal tunnel may provide temporary relief by reducing swelling around the nerve.
- Physiotherapy – Targeted exercises, nerve gliding techniques, and ergonomic advice may assist in symptom control.
When surgery may be considered
Surgery may be recommended if:
- Symptoms are severe or persistent
- There is significant weakness, muscle wasting, or loss of function
- Non-surgical options have not provided relief
The standard surgical treatment is carpal tunnel release, which involves relieving pressure on the median nerve by carefully dividing the tight ligament forming the roof of the carpal tunnel. This creates more space for the nerve and tendons.
The procedure may be performed using either an open or endoscopic (keyhole) technique, depending on the individual case. Carpal tunnel release is usually performed as a day procedure under local or general anaesthetic.
Recovery involves wound care, gradual hand exercises, and activity modification while healing takes place.
Recovery and long-term outlook
After surgery, many people experience improvement in symptoms such as night pain, numbness, and tingling. Recovery times vary, and some residual weakness or stiffness may take weeks to months to improve. Early diagnosis and treatment can help reduce the risk of permanent nerve damage.
During your consultation, Prof. Sallen will discuss the treatment options most suited to your situation, taking into account your symptoms, lifestyle, and overall health.