Shoulder Stabilisation Surgery
Comprehensive procedures to enhance shoulder stability and prevent dislocations
Shoulder stabilisation surgery is designed to treat shoulder instability, a condition that can result from trauma, repetitive movements, or congenital issues. This instability often leads to recurrent shoulder dislocations, pain, and limitations in daily activities. When conservative methods such as physical therapy or bracing are not enough, surgical intervention may be necessary to restore function and prevent further dislocations.
What is Shoulder Instability?
Shoulder instability occurs when the ball of the shoulder joint (humerus) is unable to remain in the socket (glenoid) properly. This can result from various causes, including traumatic injuries, such as dislocations, or conditions like hyperlaxity where the shoulder ligaments are too loose. Over time, instability can lead to recurrent dislocations, weakness, and pain, which can be debilitating if left untreated.
Indications for Shoulder Stabilisation Surgery
Surgical intervention for shoulder instability may be necessary when:
- The patient experiences frequent, recurrent shoulder dislocations.
- The shoulder is unstable even after non-surgical treatments, including physical therapy and bracing.
- There is significant damage to the shoulder ligaments, labrum, or bones that can’t heal on their own.
- The patient has failed conservative treatment and is unable to return to their normal activities.
Shoulder Stabilisation Procedures
Surgery may be considered when shoulder instability continues despite non-surgical treatments. The type of procedure recommended depends on the cause of instability, the extent of damage, and the individual’s activity level.
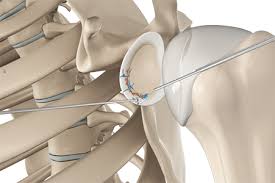
Bankart repair
This procedure is used to repair a tear of the labrum, the cartilage that helps hold the shoulder joint in place. The torn labrum is reattached to the glenoid (shoulder socket) to restore stability and reduce the chance of further dislocations. Bankart repair is often performed arthroscopically (using a minimally invasive technique).
Latarjet procedure
The Latarjet procedure may be recommended for people with significant bone loss in the shoulder socket or those who have frequent dislocations. A small piece of bone from the coracoid process is transferred to the glenoid to improve stability and prevent future dislocations.
Capsular shift (capsulorrhaphy)
In cases where the joint capsule is stretched or loose, a capsular shift can be performed. This involves tightening the capsule to limit excessive movement, supporting long-term stability and reducing the risk of repeated dislocations.
Recovery After Shoulder Stabilisation Surgery
Recovery from shoulder stabilisation surgery is a gradual process that combines rest, protection of the joint, and guided rehabilitation. The aim is to allow the repaired tissues to heal while restoring strength, movement, and stability over time.
Early phase (0–6 weeks)
The arm is usually supported in a sling to protect the repair.
Gentle hand, wrist, and elbow movements are encouraged to prevent stiffness.
Shoulder movement is generally limited, with exercises prescribed by a physiotherapist.
Intermediate phase (6–12 weeks)
The sling is gradually removed as healing progresses.
Guided physiotherapy focuses on restoring shoulder range of motion and beginning light strengthening exercises.
Daily activities can slowly be reintroduced within safe limits.
Strengthening phase (3–6 months)
Physiotherapy advances to strengthening the rotator cuff and surrounding muscles.
More demanding activities, such as lifting or light sport-specific drills, may be introduced under supervision.
Return to sport or higher-level activity (6–9 months)
Most patients can return to contact sports or heavy overhead activity only after the shoulder has regained sufficient strength, flexibility, and stability.
The exact timeline varies and is guided by the surgeon and physiotherapist.
Every recovery is individual, and progress depends on the type of procedure performed, the severity of the original injury, and the patient’s overall health and commitment to rehabilitation.

Long-Term Outcomes
Shoulder stabilisation surgery is highly successful in restoring function and preventing recurrent dislocations. With proper rehabilitation and follow-up care, most patients can return to their regular activities, including sports and exercise, with improved shoulder stability and reduced pain. The outcome of the procedure largely depends on the individual’s adherence to the rehabilitation programme and the specific type of surgery performed.
Risks and Complications
As with any surgery, shoulder stabilisation procedures carry some risks, including:
- Infection at the surgical site
- Nerve injury or damage
- Stiffness or loss of range of motion
- Recurrent instability or dislocation
- Complications related to anaesthesia
Your surgeon will discuss these risks in detail and outline the steps taken to help reduce them.
Shoulder stabilisation surgery may be considered when shoulder instability continues despite non-surgical treatments. The goal of surgery is to improve shoulder stability, reduce the likelihood of further dislocations, and restore function. The type of procedure recommended will depend on the underlying cause of instability and the individual’s needs.