Anatomical Total Shoulder Replacement (Arthroplasty)
Surgical shoulder joint replacement: restoring natural movement and alleviating arthritis pain
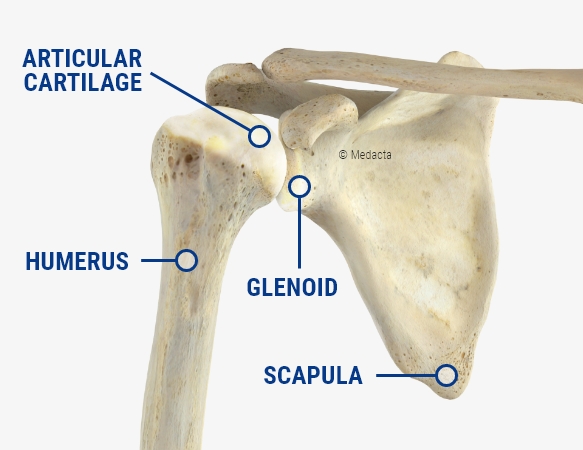
Anatomical total shoulder replacement, also known as shoulder arthroplasty, is a procedure used to replace parts of the shoulder joint that have been damaged by arthritis or injury. The operation involves replacing the ball at the top of the upper arm bone (humeral head) with a new ball made from materials such as metal, plastic, or ceramic. The socket of the joint (glenoid) is also fitted with a smooth plastic liner, allowing the ball and socket to move together more easily.
This approach is generally considered when arthritis or other conditions have significantly affected the shoulder joint but the rotator cuff tendons remain intact. The rotator cuff is essential for stabilising the shoulder, and its function supports the effectiveness and movement of the replacement joint.
Conditions That May Require an Anatomical Total Shoulder Replacement
Anatomical shoulder replacement is typically recommended for individuals experiencing:
- Osteoarthritis: The degeneration of shoulder joint cartilage, leading to pain, stiffness, and limited movement.
- Rheumatoid Arthritis: Inflammatory arthritis that damages the shoulder joint, causing pain and swelling.
- Severe Fractures: Complex shoulder fractures that necessitate joint replacement if they cannot be repaired.
- Avascular Necrosis: A lack of blood supply to the humeral head, resulting in bone death and joint collapse, making replacement necessary.
To assess whether an anatomical total shoulder replacement is appropriate, Melbourne Orthopaedic Clinic, will conduct a thorough examination and review your symptoms, including an assessment of your shoulder’s range of motion and strength.
Imaging tests play a vital role in diagnosing the extent of joint damage:
- X-rays: Help determine the degree of cartilage loss, joint space narrowing, and bone damage.
- MRI or CT scan: These advanced imaging techniques provide detailed views of the bones, cartilage, and surrounding soft tissues, including the rotator cuff, ensuring an appropriate treatment plan.
Patients with an intact rotator cuff and significant pain or functional limitations that haven’t improved with non-surgical treatments are the best candidates for this procedure.
The Anatomical Shoulder Replacement Surgical Procedure
Anaesthesia and Surgical Preparation
Anatomical shoulder replacement is generally performed under either general anaesthesia or regional anaesthesia (nerve block), depending on individual circumstances and preferences. General anaesthesia keeps you asleep during the procedure, while a nerve block numbs the shoulder and arm area, often combined with sedation for comfort. Melbourne Orthopaedic Clinic surgeons and the anaesthesia team will determine the best option based on your health and comfort.
Once anaesthesia is administered, the surgical team will position your shoulder for optimal access to the joint. A sterilised area will be prepared before the procedure commences.
Removal of Damaged Joint Parts
The initial step involves accessing the shoulder joint through a carefully placed incision, typically on the front or side of the shoulder. Melbourne Orthopaedic Clinic, will meticulously remove any damaged or worn components of the shoulder joint, including the humeral head (the ball of the upper arm bone) and, if needed, the glenoid (the socket of the shoulder blade). This may also involve the removal of bone spurs or worn areas of cartilage due to arthritis, which contribute to pain and limited movement.
Replacing the Humeral Head
After removing the damaged humeral head, it is replaced with a prosthetic ball made of metal or ceramic. This prosthesis is designed to mimic the natural ball of the upper arm bone and is securely attached to the bone. Typically, the upper part of the humerus (the arm bone) is prepared to fit a stem that is inserted into the bone, holding the prosthetic ball in place for stability and durability. The choice of material (metal or ceramic) is based on its strength and compatibility with the body.
Replacing the Glenoid (Shoulder Socket)
Next, attention is turned to the glenoid socket. The glenoid, the shallow socket of the shoulder blade, will receive a plastic liner after any damaged cartilage or bone is removed. This liner is affixed using medical-grade cement or screws, depending on the bone condition. The liner provides a smooth surface that interacts with the new humeral head, facilitating fluid movement and minimising friction within the joint.
Preservation of the Rotator Cuff
A critical aspect of a successful anatomical total shoulder replacement is maintaining the integrity of the rotator cuff muscles. These muscles and tendons surround the shoulder joint, stabilising and controlling its movement. During the procedure Melbourne Orthopaedic Clinic will take care to preserve these muscles, which are vital for keeping the new ball securely in the socket after the replacement. If the rotator cuff is intact and functional prior to surgery, it will continue to provide stability for the new joint, allowing for smoother movement and reduced wear on the prosthetic components.
Closing the Incision and Immediate Post-Operative Care
Once the prosthetic components are securely in place and the joint is properly aligned and stable, Melbourne Orthopaedic Clinic will close the incision with sutures or staples, followed by applying a sterile dressing to protect the wound.
Immediately following the procedure, a sling or shoulder immobiliser will be fitted to keep the arm in place, allowing the new joint to begin healing. The team at Melbourne Orthopaedic Clinic will monitor you in the recovery room to ensure comfort and a smooth recovery from anaesthesia. You will also receive instructions for post-operative care, including pain management and when to start the initial stages of rehabilitation.
Recovery and Rehabilitation Following Anatomical Total Shoulder Replacement
Recovering from an anatomical total shoulder replacement is a gradual process requiring commitment to post-operative care and rehabilitation to achieve the best possible outcome. Recovery timelines can vary based on overall health, adherence to the rehabilitation plan, and the condition of the shoulder prior to surgery. Below is a general guide for what to expect in the weeks and months following surgery.
Immediate Post-Operative Period: First 1-2 Weeks
- Hospital Stay: After surgery, you may stay in the hospital for one to two nights, depending on your recovery. During this period, the medical team will monitor your pain, assist with discomfort management, and ensure the shoulder is protected in a sling. Some patients may be discharged the same day, based on the surgery’s complexity and your individual case.
- Immobilisation and Sling Use: For the first few weeks post-surgery, wearing a sling or shoulder immobiliser is essential to protect the shoulder and allow for proper healing. The sling keeps your arm close to your body, preventing movements that could disrupt healing. It is crucial to wear the sling at all times, even while sleeping, unless otherwise instructed by Melbourne Orthopaedic Clinic or your physiotherapist.
- Pain Management: Post-operative pain is common but typically improves within the first few days. Pain management includes prescribed medications, such as anti-inflammatories and pain relievers. Applying ice packs and keeping your arm elevated as directed can help reduce swelling and discomfort.
Early Rehabilitation: 2-6 Weeks
- Gentle Passive Movements: Within the first two weeks, your physiotherapist will guide you through passive range-of-motion exercises, where they gently move your arm for you. These exercises maintain mobility in the shoulder joint without straining your muscles. It’s important to follow your physiotherapist’s guidance to avoid stressing the joint prematurely.
- Restrictions: Active use of the shoulder should be avoided during this period. Refrain from lifting, pushing, pulling, and reaching overhead to protect the healing tissues. Adhere to the specific restrictions provided by your surgeon and physiotherapist for the best results.
Intermediate Rehabilitation: 6-12 Weeks
- Transition to Active Motion: By six weeks post-surgery, most patients begin active range-of-motion exercises, allowing for self-movement within a controlled program. This phase aims to restore mobility and gradually improve shoulder function without compromising healing.
- Weaning off the Sling: Around six to eight weeks after surgery, you may start to wean off the sling as directed by your physiotherapist. Light daily activities, such as dressing or eating, can be resumed, but heavy lifting and strenuous tasks should still be avoided.
- Strengthening Exercises: At this stage, you will begin strengthening exercises to rebuild the muscles surrounding the shoulder, particularly the rotator cuff and scapular stabilisers. These exercises will be performed gently and gradually, focusing on regaining muscle strength and endurance while protecting the joint.
Late Rehabilitation: 3-6 Months
- Regaining Full Range of Motion: By three months post-surgery, most patients notice significant improvements in range of motion and strength. Your physiotherapist will guide you through more challenging exercises to enhance flexibility, stability, and overall shoulder function. However, avoid heavy lifting and high-impact activities during this period.
- Return to Daily Activities: Around four to six months post-surgery, many patients can return to light to moderate activities, including household tasks, driving, and low-impact exercises like walking or stationary cycling. You’ll continue to gain strength, with a noticeable reduction in pain compared to pre-surgery levels.
Full Recovery: 6-12 Months
- Return to Sports and Hobbies: By six to nine months after surgery, most patients can resume activities like swimming, golf, or gardening. However, high-impact sports and activities involving heavy lifting may need to be postponed until nine to twelve months, based on your progress and Melbourne Orthopaedic Clinic guidance.
- Ongoing Strength and Mobility Improvements: Full recovery can take up to twelve months, during which you may continue experiencing gradual improvements in strength, mobility, and endurance. Regular physiotherapy and home exercises remain crucial for optimising shoulder function and maintaining flexibility. While complete range of motion may not fully return to pre-arthritis levels, most patients report significant pain relief and an improved ability to perform daily activities.
Long-Term Outlook
Anatomical shoulder replacement boasts a high success rate, enabling many individuals to resume their daily activities and hobbies without significant pain. Long-term outcomes are often excellent, with improvements in pain management and joint function lasting for years.
Maintaining a healthy lifestyle, including regular exercise and a balanced diet, can significantly impact your long-term shoulder health and overall well-being. Always consult Melbourne Orthopaedic Clinic regarding any concerns about your shoulder or any changes in pain or mobility after surgery.

Potential Risks And Outcomes For Anatomical Total Shoulder Replacement Surgery
As with any surgical procedure, there are risks associated with shoulder replacement surgery, including infection, blood clots, or complications with the prosthetic components. Shoulder replacements do however have a high success rate when performed by experienced surgeons.
The primary aim of anatomical shoulder replacement is to significantly alleviate pain and enhance function. While some patients may experience persistent limitations in their range of motion, the majority report a marked improvement in their quality of life, enabling them to engage in daily activities without pain.
Anatomical total shoulder replacement can significantly enhance the quality of life for individuals suffering from severe shoulder pain due to arthritis or joint damage. By restoring the normal function of the shoulder joint, patients can enjoy increased mobility and reduced pain, allowing them to return to daily activities and hobbies. Melbourne Orthopaedic Clinic is committed to providing comprehensive care throughout the surgical and recovery process, ensuring the best possible outcomes for all patients.