Spondylolisthesis
A condition characterised by the slipping of one vertebra over another
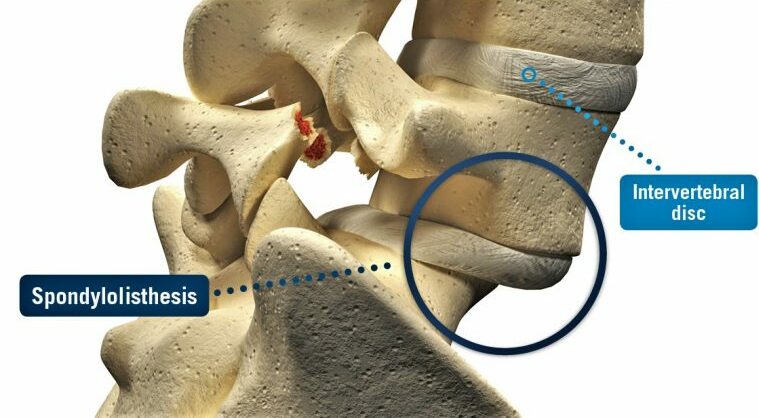
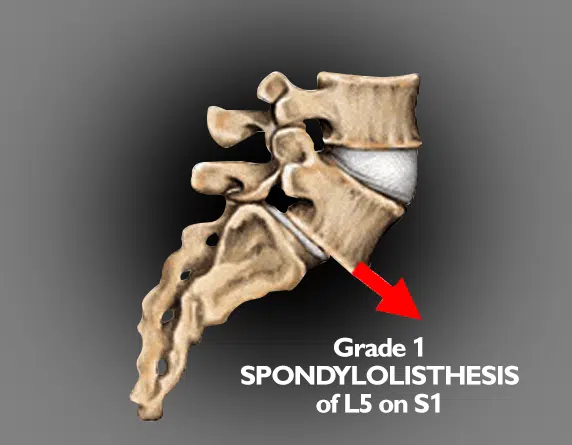
Spondylolisthesis is a condition where one vertebra slips forward over the one beneath it. This can occur in any part of the spine but is most commonly seen in the lower back (lumbar region). The slippage may create spinal instability and, in some cases, place pressure on nearby nerves.
Causes of spondylolisthesis can include congenital defects in the spine, gradual degenerative changes related to ageing, stress fractures from repetitive strain, or trauma. Symptoms vary widely, from mild back discomfort to more significant pain, stiffness, or nerve-related issues such as tingling or weakness in the legs.
Management depends on the severity of the slip, the presence of nerve involvement, and how much the condition affects daily function.
Causes of Spondylolisthesis
Several factors can contribute to the development of spondylolisthesis, including:
- Degenerative Changes: Age-related wear and tear on the spinal discs and joints can lead to instability, allowing the vertebrae to slip.
- Congenital Defects: Some individuals are born with a defect in the spine that predisposes them to spondylolisthesis.
- Trauma or Injury: Fractures or injuries to the spine can disrupt the alignment of the vertebrae.
- Repetitive Stress: Activities that place excessive stress on the spine, such as certain sports or manual labour, can contribute to the condition.
- Obesity: Excess weight can place additional strain on the spine, increasing the risk of spondylolisthesis.
Symptoms of Spondylolisthesis
The symptoms of spondylolisthesis can vary widely depending on the severity of the condition but commonly include:
- Lower Back Pain: Pain in the lower back, which may worsen with activity or prolonged sitting.
- Leg Pain: Radiating pain in the legs, often similar to sciatica, may occur if nerve roots are compressed.
- Muscle Weakness: Weakness or numbness in the legs or feet, particularly with prolonged standing or walking.
- Postural Changes: A noticeable change in posture or gait due to pain and discomfort.
Diagnosis of Spondylolisthesis
Diagnosis usually begins with a medical history and physical examination. Prof. Hunt will ask about back pain, leg pain, stiffness, or neurological symptoms such as tingling or weakness. He may also assess posture, gait, and spinal flexibility to look for signs of instability.
Physical examination
- Observation for changes in spinal alignment or curvature.
- Palpation of the spine to detect step-offs (where one vertebra feels forward compared to another).
- Neurological assessment of reflexes, strength, and sensation to check for nerve involvement.
Imaging tests
Imaging is used to confirm the diagnosis and assess the severity of slippage:
- X-rays – The primary test for detecting vertebral slippage and measuring its degree. Standing X-rays may show instability when bending forward or backward.
- Magnetic resonance imaging (MRI) – Provides detailed views of the spinal cord, nerves, and discs, helping to identify compression or related soft tissue problems.
- Computed tomography (CT) scan – May be used for more detailed bone assessment, particularly if surgery is being considered.
The combination of clinical examination and imaging helps determine the type and severity of spondylolisthesis, guiding the most appropriate treatment plan.
Treatment Options for Spondylolisthesis
Treatment for spondylolisthesis depends on the degree of vertebral slippage, the severity of symptoms, and whether there is nerve involvement. The main goals are to reduce pain, improve mobility, and stabilise the spine.
Non-surgical treatments
Many people find improvement with non-surgical management, which may include:
- Physiotherapy – Strengthening the core and back muscles, improving posture, and increasing flexibility can help support the spine and reduce symptoms.
- Medications – Non-steroidal anti-inflammatory drugs (NSAIDs) and other pain relief options may be used to manage discomfort.
- Activity modification – Avoiding activities that worsen symptoms, while maintaining gentle, low-impact exercise such as walking or swimming.
- Bracing – In some cases, especially in younger patients, a brace may be used to limit excessive spinal motion and provide support.
- Epidural steroid injections – May be used to reduce inflammation and relieve nerve-related pain.
Surgical treatments
Surgery may be considered if symptoms persist despite conservative care, if there is significant nerve compression, or if the vertebral slippage is severe. Options include:
- Spinal decompression – Removal of bone or tissue pressing on the nerves.
- Spinal fusion – Joining two or more vertebrae together using bone grafts and instrumentation (such as screws and rods) to stabilise the spine. This is often combined with decompression if nerve pressure is present.
The choice of treatment is individual and guided by the type of spondylolisthesis, the degree of slippage, and the patient’s overall health and activity goals.