Lumbar Spinal Stenosis
A condition characterised by narrowing of the spinal canal
Spinal stenosis occurs when the spinal canal becomes narrowed, placing pressure on the spinal cord and surrounding nerves. This narrowing can happen in different parts of the spine and is often linked to age-related changes such as degenerative disc disease, thickened ligaments, or osteoarthritis.
Symptoms vary depending on the location and severity of the narrowing. They may include pain, tingling, numbness, or weakness in the arms or legs, and in some cases difficulty with walking or balance.
Spinal stenosis can range from mild to more severe, and treatment options depend on how much it affects daily activities and overall function. Management may include physiotherapy, medications, or surgical procedures if non-surgical care does not provide enough relief.

Causes of Spinal Stenosis
Several factors can contribute to the development of spinal stenosis, including:
- Degenerative Changes: The natural ageing process can lead to degenerative changes in the spine, such as disc degeneration, which can contribute to narrowing of the spinal canal.
- Bone Spurs: The formation of bone spurs, or osteophytes, can occur as the body responds to degenerative changes, further constricting the space for the spinal cord and nerves.
- Thickened Ligaments: The ligaments in the spine can become thickened or calcified, leading to a reduction in space within the spinal canal.
- Herniated Discs: Bulging or herniated discs can protrude into the spinal canal, exerting pressure on nearby nerves and contributing to stenosis.
- Congenital Conditions: Some individuals may be born with a naturally narrow spinal canal, making them more susceptible to spinal stenosis.
Symptoms of Spinal Stenosis
Symptoms of spinal stenosis can vary widely but may include:
- Pain: Chronic pain in the neck or lower back, often aggravated by prolonged standing or walking.
- Numbness and Tingling: Sensations of numbness, tingling, or weakness in the legs, arms, or hands, depending on the location of the stenosis.
- Claudication: Pain or cramping in the legs that occurs during physical activity and improves with rest.
- Balance Issues: Difficulty with balance and coordination, leading to an increased risk of falls.
Diagnosis of Spinal Stenosis
Diagnosing spinal stenosis usually begins with a detailed discussion of symptoms and a physical examination. Your surgeon may check for signs such as muscle weakness, changes in reflexes, numbness, or difficulty with walking and balance.
Imaging tests
To confirm the diagnosis and assess the severity of the narrowing, imaging may be recommended:
- X-rays – Can show changes in bone structure, such as arthritis, bone spurs, or reduced disc height.
- Magnetic resonance imaging (MRI) – Provides detailed images of soft tissues, including discs, ligaments, and nerves, and is commonly used to identify the location and extent of narrowing.
- Computed tomography (CT) scan – Produces cross-sectional images of the spine and may be used if MRI is not suitable.
- CT myelogram – Involves injecting contrast dye into the spinal canal before a CT scan to highlight areas of nerve compression.
Neurological tests
In some cases, nerve studies such as electromyography (EMG) may be performed to measure electrical activity in the muscles and help determine which nerves are affected.
The combination of a physical assessment and imaging helps guide an appropriate treatment plan tailored to the individual’s needs and symptoms.
Spinal Stenosis Treatment Options
Treatment for spinal stenosis focuses on relieving pressure on the nerves, reducing pain, and improving mobility. The best approach depends on the severity of symptoms, the location of the narrowing, and how much it interferes with daily activities.
Non-surgical treatments
Many people manage spinal stenosis with non-surgical options, including:
- Physiotherapy – Exercises to strengthen supporting muscles, improve posture, and increase flexibility can reduce strain on the spine and ease symptoms.
- Medications – Anti-inflammatory drugs (NSAIDs), pain relievers, or muscle relaxants may help manage discomfort.
- Epidural steroid injections – Corticosteroid injections can reduce inflammation and swelling around the nerves, providing temporary relief.
- Activity modification – Avoiding movements that worsen symptoms, combined with low-impact exercise such as walking, cycling, or swimming, may help maintain mobility.
Surgical treatments
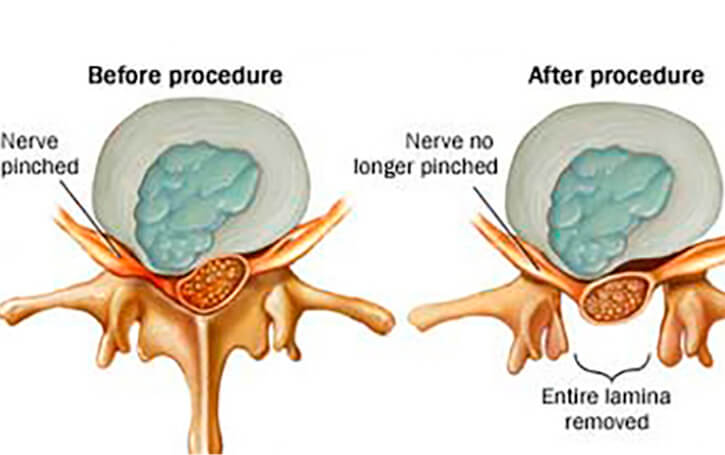
If non-surgical measures do not provide sufficient relief, surgery may be considered to create more space within the spinal canal and reduce nerve compression. Common procedures include:
- Laminectomy – Removal of part of the vertebra (lamina) to relieve pressure on the spinal cord or nerves.
- Laminotomy – Partial removal of the lamina to enlarge the spinal canal while preserving more of the bone structure.
- Foraminotomy – Widening of the openings (foramina) where nerves exit the spinal canal, reducing compression.
- Spinal fusion – In some cases, fusion may be performed alongside decompression surgery to stabilise the spine.
The choice of treatment is individual and depends on the patient’s symptoms, general health, and treatment goals.