Kyphosis
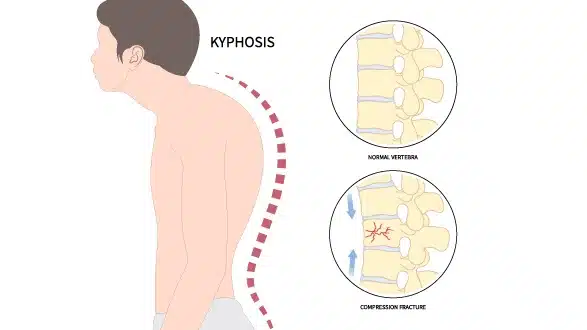
A condition characterised by an abnormal forward curvature of the spine
Kyphosis is a spinal condition characterised by an exaggerated forward curve of the upper back, sometimes described as a rounded or hunched posture. While some curvature in the thoracic spine is normal, excessive curvature may cause back pain, stiffness, reduced mobility, or visible changes in posture.
Kyphosis can occur at any age. In younger people it may result from conditions such as Scheuermann’s disease or congenital spinal differences, while in older adults it is more often linked to degenerative changes, osteoporosis, or vertebral fractures.
The impact of kyphosis varies. Some cases cause minimal symptoms, while more severe curvature can affect breathing, balance, or overall function. Management depends on the underlying cause, the degree of curvature, and the severity of symptoms, and may include physiotherapy, bracing, or surgery in selected cases.
.
Causes of Kyphosis
Kyphosis can develop from a range of underlying factors that affect the structure and strength of the spine. Common causes include:
- Postural kyphosis – Often seen in adolescents and young adults, this type develops from poor posture, muscle weakness, or prolonged slouching. It usually improves with exercises and postural correction.
- Scheuermann’s disease – A developmental condition in teenagers where the vertebrae grow unevenly, leading to wedge-shaped bones and a more pronounced curve.
- Congenital kyphosis – Present at birth, caused by abnormal spinal development in the womb. The curvature often worsens as the child grows.
- Osteoporosis – Weakening of the bones in older adults can cause compression fractures in the vertebrae, resulting in increased curvature.
- Degenerative changes – Age-related wear and tear on the discs and joints of the spine can gradually alter spinal alignment.
- Trauma – Fractures or injuries to the spine may lead to abnormal curvature.
- Other medical conditions – Disorders such as spinal infections, tumours, or neuromuscular diseases (e.g., muscular dystrophy) may also contribute.
The cause of kyphosis helps determine the most appropriate treatment, which may range from observation and physiotherapy to bracing or surgery in more severe cases.
Symptoms of Kyphosis
The symptoms of kyphosis can vary depending on the severity of the curvature and its underlying cause. Some people experience few or no symptoms, while others may notice pain or changes in posture that affect daily activities. Common symptoms include:
- Visible curvature – A rounded or hunched appearance of the upper back, often more noticeable when standing or sitting upright.
- Back pain or stiffness – Discomfort in the upper or mid-back, which may worsen after long periods of sitting or standing.
- Reduced mobility – Difficulty straightening the spine fully or maintaining good posture.
- Muscle fatigue – Strain in the back and shoulder muscles from supporting the altered posture.
- Height loss – In some cases, particularly in older adults, progressive curvature can make a person appear shorter.
- Neurological symptoms – In severe cases, compression of nerves may lead to tingling, numbness, or weakness in the arms or legs.
- Breathing difficulties – Rarely, very pronounced curvature can restrict lung expansion and affect breathing.
Symptoms may progress gradually, especially in age-related kyphosis, and early assessment can help guide treatment and prevent worsening of the curve.
Diagnosis of Kyphosis
Diagnosis of kyphosis usually begins with a medical history and physical examination. Your doctor will ask about symptoms such as back pain, stiffness, or changes in posture, as well as any relevant family or medical history.
Physical examination
Observation of the spine from the side to assess the degree of curvature.
Postural assessment while standing and bending forward.
Palpation of the spine to detect any irregularities in the vertebrae.
Neurological checks, including reflexes, strength, and sensation, if nerve involvement is suspected.
Imaging tests
To confirm the diagnosis and measure the extent of curvature, imaging may be recommended:
X-rays – The most common test, used to measure the angle of curvature (Cobb angle) and determine severity.
Magnetic resonance imaging (MRI) – Provides detailed images of discs, spinal cord, and nerves, and may be used if neurological symptoms are present.
Computed tomography (CT) scan – Can give additional detail about bone structure, especially in cases of trauma or complex deformities.
The findings from the physical examination and imaging help determine the type of kyphosis, its severity, and the most suitable treatment approach.
Kyphosis Treatment Options
The management of kyphosis depends on the underlying cause, the severity of the curve, symptoms, and the patient’s age. Some cases require only observation, while others may benefit from physiotherapy, bracing, or surgery.
Non-surgical treatments
Observation and monitoring – For mild curves without significant symptoms, regular check-ups and imaging may be recommended to track progression.
Physiotherapy – Strengthening and stretching exercises can improve posture, reduce discomfort, and support spinal alignment.
Bracing – In adolescents with Scheuermann’s disease or progressing curvature, a spinal brace may be prescribed to help prevent further worsening while the spine is still growing.
Medications – Pain relief or anti-inflammatory medicines may help manage discomfort.
Lifestyle modifications – Posture correction, ergonomic adjustments, and low-impact exercise may help reduce strain on the spine.
Surgical treatments
Surgery may be considered in more severe cases, particularly when:
The curvature is pronounced and continues to worsen.
Pain or neurological symptoms significantly impact daily life.
Breathing or organ function is affected by the spinal deformity.
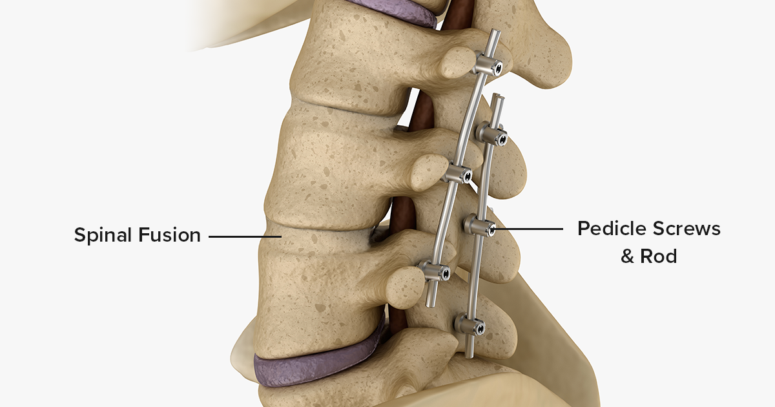
The most common procedure is spinal fusion, where vertebrae are stabilised using rods, screws, and bone grafts to correct and support the curve.
The decision to proceed with surgery is made on an individual basis, taking into account the severity of the curve, overall health, and patient goals.