Herniated Disc (Slipped Disc)
A common spine condition leading to pain and discomfort
A herniated disc, sometimes called a slipped disc, occurs when the soft inner material of a spinal disc pushes through a tear in its tougher outer layer. This can put pressure on nearby nerves and may cause pain, numbness, or weakness in the arms or legs, depending on where the disc is affected.
Herniated discs can develop anywhere along the spine but are most common in the lower back (lumbar region) and the neck (cervical region). Symptoms and their severity vary from person to person, and treatment options depend on the location and impact of the herniation.
Causes of Herniated Discs
Herniated discs can result from various factors, including:
- Age-Related Degeneration: As we age, the spinal discs lose hydration and elasticity, making them more susceptible to damage.
- Repetitive Strain: Engaging in activities that involve heavy lifting or repetitive twisting motions can increase the risk of a disc herniation.
- Trauma or Injury: Accidents, falls, or sports injuries can lead to sudden disc herniation.
- Genetic Predisposition: Some individuals may inherit a tendency to develop disc problems due to genetic factors.
- Sedentary Lifestyle: Poor posture and lack of regular exercise can weaken the muscles supporting the spine, contributing to disc issues.
Symptoms of Herniated Discs
The symptoms of a herniated disc can vary depending on the severity of the herniation and its location. Common symptoms include:
- Pain: Localised pain in the back or neck, which may radiate down the arms or legs, often described as sharp, burning, or shooting pain.
- Numbness or Tingling: Individuals may experience numbness or tingling sensations in the affected limbs, indicating nerve involvement.
- Muscle Weakness: Weakness in the muscles of the arms or legs, making it difficult to perform everyday activities.
- Loss of Reflexes: Reduced reflex responses in the affected areas may also be present.
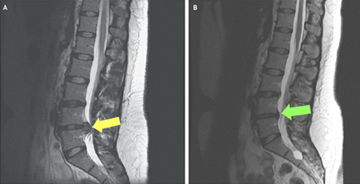
Diagnosis of Herniated Discs
Diagnosing a herniated disc begins with a detailed medical history and physical examination. Your doctor will ask about your symptoms, such as pain, numbness, weakness, or changes in mobility, and may check your reflexes, muscle strength, and range of motion.
Imaging tests
If a herniated disc is suspected, imaging may be used to confirm the diagnosis and assess its severity:
- X-rays – While X-rays cannot show a herniated disc directly, they can help rule out other causes of back or neck pain, such as fractures or arthritis.
- Magnetic resonance imaging (MRI) – MRI scans provide clear images of soft tissues, including discs and nerves, and are the most common test used to confirm a disc herniation.
- Computed tomography (CT) scan – CT scans can give detailed cross-sectional images of the spine and may be used if MRI is not suitable.
- Myelogram – In some cases, dye is injected into the spinal canal before a CT scan to highlight pressure on the spinal cord or nerves.
Nerve tests
Electromyography (EMG) and nerve conduction studies may also be recommended to measure electrical activity in the muscles and nerves, helping to identify the specific nerves being affected by the herniation.
The combination of physical examination and imaging helps guide an appropriate treatment plan tailored to the individual’s symptoms and condition.
Treatment Options for Herniated Disc
Treatment for a herniated disc usually aims to relieve pain, reduce inflammation, and restore normal movement and function. The choice of treatment depends on the severity of symptoms, the location of the herniation, and how it affects daily life.
Non-surgical treatments
Many people improve with non-surgical management, which may include:
- Physiotherapy – A physiotherapist may recommend exercises to strengthen supporting muscles, improve flexibility, and help manage pain.
- Medications – Anti-inflammatory medicines (NSAIDs) or muscle relaxants may be prescribed to reduce pain and inflammation.
- Epidural steroid injections – In some cases, corticosteroid injections are used to target swelling and irritation around the affected nerves.
- Activity modification – Adjusting or avoiding activities that aggravate symptoms, combined with low-impact exercise, can support recovery.
Surgical treatments
If symptoms persist despite non-surgical care, surgery may be considered. Options include:
- Discectomy – Removal of the herniated portion of the disc to relieve pressure on nearby nerves.
- Laminectomy – Removal of part of the vertebra to create more space in the spinal canal and reduce nerve compression.
Every treatment plan is individual, and Prof. Justin Hunt will discuss the potential benefits and risks of each option to help determine the most appropriate approach.