Ankylosing Spondylitis
A chronic inflammatory condition primarily affecting the spine
Ankylosing spondylitis (AS) is a long-term inflammatory condition that mainly affects the spine and the sacroiliac joints, where the spine meets the pelvis. It often causes pain and stiffness in the back and hips, which may worsen after rest or inactivity.
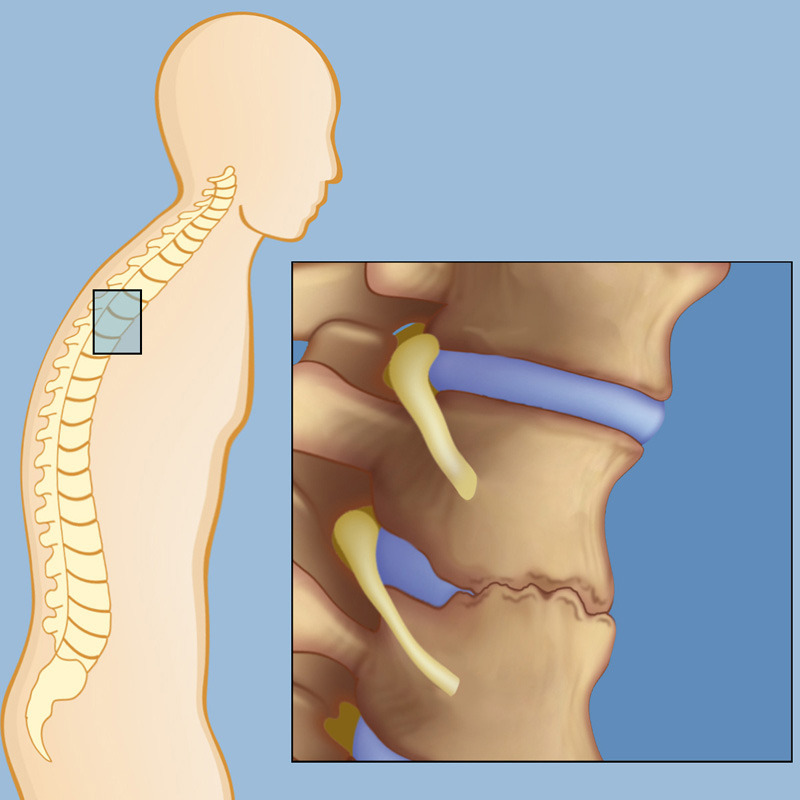
Over time, ongoing inflammation can lead to new bone formation between the vertebrae, causing parts of the spine to fuse. This may result in reduced flexibility and, in more advanced cases, a forward-stooped posture.
Although AS can occur in anyone, it is more common in men and usually develops in late adolescence or early adulthood. The severity and progression of the condition vary from person to person, and early diagnosis and management are important to help maintain mobility and manage symptoms.
Causes of Ankylosing Spondylitis
The exact cause of ankylosing spondylitis (AS) is not fully understood, but research suggests it develops from a combination of genetic and environmental factors.
- Genetics – The strongest risk factor is the presence of a gene called HLA-B27. Many people with AS carry this gene, although not everyone with HLA-B27 develops the condition. Other genes may also play a role.
- Immune system response – AS is an inflammatory condition thought to involve an abnormal immune response. The immune system mistakenly triggers inflammation in the joints of the spine and pelvis.
- Environmental triggers – Factors such as infections may contribute to the onset of the condition in people who are genetically predisposed, although the exact triggers are not clear.
- Family history – People with a close relative who has AS are at higher risk of developing the condition themselves.
While the precise cause remains uncertain, understanding these contributing factors helps guide research and management of the condition.
.
Symptoms of Ankylosing Spondylitis
The symptoms of ankylosing spondylitis (AS) can vary widely between individuals, but most people experience gradual onset of back pain and stiffness. Symptoms often begin in the late teens or early adulthood and may develop slowly over time.
Common features include:
- Chronic back pain and stiffness – Typically worse in the morning or after periods of rest and often improves with movement and exercise.
- Hip and buttock pain – Pain in the sacroiliac joints, where the spine meets the pelvis, is common.
- Reduced flexibility – Ongoing inflammation can limit movement in the spine, making it harder to bend or twist.
- Fatigue – Persistent inflammation can contribute to tiredness and low energy levels.
- Postural changes – In advanced cases, new bone formation between vertebrae may cause the spine to stiffen and lead to a forward-stooped posture.
Other symptoms may include pain or stiffness in areas outside the spine, such as the shoulders, ribs, or heels. Some individuals also experience inflammation in the eyes (uveitis), which can cause redness, pain, and sensitivity to light.
Diagnosis of Ankylosing Spondylitis
Diagnosing ankylosing spondylitis (AS) can be challenging because early symptoms such as back pain and stiffness are common to many other conditions. A combination of medical history, physical examination, imaging, and laboratory tests is usually needed to confirm the diagnosis.
Medical history and physical examination
Your doctor will ask about the nature and duration of symptoms, including whether back pain improves with activity or worsens after rest.
A physical examination may assess spinal flexibility, posture, and areas of tenderness, as well as hip and sacroiliac joint involvement.
Imaging tests
X-rays – Can show characteristic changes in the sacroiliac joints and spine, although these may take years to appear.
Magnetic resonance imaging (MRI) – Detects early signs of inflammation in the sacroiliac joints and spine, making it useful for diagnosing AS before changes are visible on X-ray.
Computed tomography (CT) scan – Sometimes used to provide detailed images of joint and bone structure.
Laboratory tests
Blood tests may be used to check for markers of inflammation, such as C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR).
Genetic testing for the HLA-B27 gene may be performed, as its presence increases the likelihood of AS, though not all people with the gene will develop the condition.
A confirmed diagnosis usually requires evidence of both clinical features (such as inflammatory back pain) and objective findings from imaging or lab tests.
Treatment Options for Ankylosing Spondylitis
Ankylosing spondylitis (AS) is a long-term condition, and while it cannot be cured, treatment aims to manage symptoms, reduce inflammation, and preserve mobility. The best approach depends on the severity of symptoms, the degree of spinal involvement, and the individual’s overall health.
Non-surgical treatments
Physiotherapy and exercise – Regular movement and tailored physiotherapy programs are central to managing AS. Exercises focus on posture, spinal flexibility, breathing capacity, and strengthening supportive muscles.
Medications –
Non-steroidal anti-inflammatory drugs (NSAIDs) are often the first-line treatment to reduce pain and inflammation.
Disease-modifying anti-rheumatic drugs (DMARDs) may be used if peripheral joints (outside the spine) are affected.
Biologic therapies (e.g., TNF inhibitors or IL-17 inhibitors) may be considered for individuals with persistent symptoms who do not respond adequately to standard treatments.
Lifestyle modifications – Activities such as swimming, yoga, or low-impact exercise can help maintain flexibility. Avoiding smoking and maintaining a healthy weight also support spinal health.
Pain management techniques – Heat therapy, posture training, and pacing of activities can help relieve discomfort.
Surgical treatments
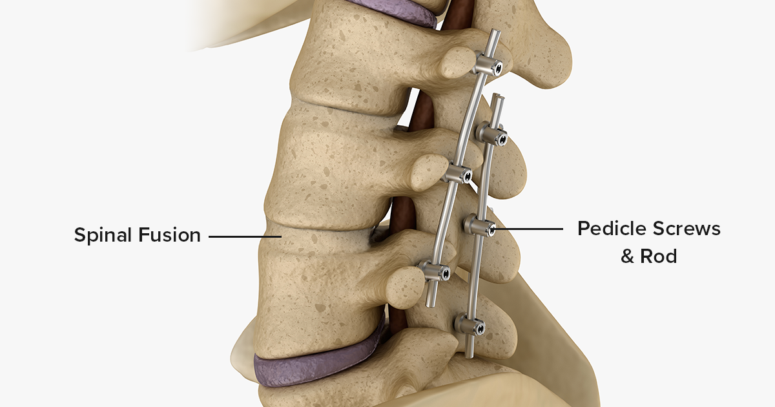
Surgery is rarely required for ankylosing spondylitis, but may be considered if there is severe joint damage, spinal deformity, or nerve compression. Options include:
Joint replacement surgery – For severe hip or shoulder involvement.
Corrective spinal surgery – In selected cases with significant deformity affecting function or quality of life.
The treatment plan is tailored to the individual, and ongoing monitoring is important to adjust care as the condition progresses.